Anyone who has seen a decrease, shout it out, along with your regimen.
Measured from 4.8 up to 6.2%. In average 5.1% during the last 9 years. But there is a problem with HbA1c, in that it depends for example on the clearing rate of RBC - usually about 3 months - and other factors. With a faster clearing rate or a high vitamin C intake it shows a lowered value.
Journal of the New Zealand Medical Association, 23-August-2002, Vol 115 No 1160
Glycohaemoglobin and ascorbic acid
Copplestone et al1 (http://www.nzma.org....al/115-1157/25/) identified misleading glycohaemoglobin (GHb) results due to a haemoglobin variant (Hb D Punjab) and listed a number of other possible causes for such false results (ie, haemolytic anaemia, uraemia, lead poisoning, alcoholism, high-dose salicylates and hereditary persistence of foetal haemoglobin).
We have observed a significant "false" lowering of GHb in animals and humans supplementing ascorbic acid (AA) at multigram levels. Mice receiving ~7.5 mg/d (equivalent to > 10 g/day in a 70 kg human) exhibited no decrease in plasma glucose, but a 23% reduction in GHb.2 In humans, supplementation of AA for several months did not lower fasting plasma glucose.3,4 We studied 139 consecutive consenting non-diabetic patients in an oncology clinic. The patients had been encouraged as part of their treatment to supplement AA. Self-reported daily intake varied from 0 to 20 g/day. The plasma AA levels ranged from 11.4 to 517 µmol/L and correlated well with the reported intake. Regression analysis of their GHb and plasma AA values showed a statistically significant inverse association (eg, each 30 µmol/L increase in plasma AA concentration resulted in a decrease of 0.1 in GHb).
A 1 g oral dose of AA can raise plasma AA to 130 µmol/L within an hour and such doses at intervals of about two hours throughout the day can maintain ~230 µmol AA/L.5 Similar levels could also be achieved by use of sustained-release AA tablets. This AA concentration would induce an approximate 0.7 depression in GHb. The GHb assay used in our study, affinity chromatography, is not affected by the presence of AA.3 Thus, unlike the case with Hb D Punjab, our results were not caused by analytical method artifact. More likely, the decreased GHb associated with AA supplementation appears related to an in vivo inhibition of glycation by the elevated plasma AA levels, and not a decrease in average plasma glucose.3 If this is true, the effect has implications not only for interpretation of GHb but also for human ageing, in which glycation of proteins plays a prominent role in age-related degenerative changes.
A misleading GHb lowering of the magnitude we observed can be clinically significant. Current recommendations for diabetics suggest that GHb be maintained at 7, a level that is associated with acceptable control and decreased risk of complications; when GHb exceeds 8, re-evaluation of treatment is necessary.6 Moreover, relatively small increases in average blood sugar (ie, GHb) can accompany adverse reproductive effects. A difference in mean maternal GHb of 0.8 was found for women giving birth to infants without or with congenital malformations.7 In either of these circumstances, an underestimation of GHb could obscure the need for more aggressive intervention.
Vitamin usage is common in New Zealand and after multivitamins, AA is the most often consumed supplement.8 Moreover, diabetics are encouraged to supplement antioxidants, including AA. Thus, it seems prudent for primary care health providers to inquire regarding the AA intake of patients, especially diabetics, when using GHb for diagnosis or treatment monitoring.
Cheryl A Krone
Senior Research Scientist
John TA Ely
Director
Applied Research Institute
PO Box 1925
Palmerston North
References:
- Copplestone S, Mackay R, Brennan S. Normal glycated haemoglobin in a patient with poorly controlled diabetes mellitus and haemoglobin D Punjab: implications for assessment of control. NZ Med J 2002;115(1157). URL: http://www.nzma.org....al/115-1157/25/
- Krone CA, Ely JTA. Vitamin C and glycohemoglobin revisited. Clin Chem 2001;47(1):148.
- Davie SJ, Gould BJ, Yudkin JS. Effect of vitamin C on glycosylation of proteins. Diabetes 1992;41(2):167–73.
- Paolisso G, Balbi V, Bolpe C, et al. Metabolic benefits deriving from chronic vitamin C supplementation in aged non-insulin dependent diabetics. J Am Coll Nutr 1995; 14(4):387–392.
- Lewin S. Vitamin C: Its Molecular Biology and Medical Potential. New York: Academic Press; 1976.
- Kenealey T, Braatvedt G, Scragg R. Screening for type 2 diabetes in non-pregnant adults in New Zealand: practice recommendations. NZ Med J 2002;115(1152):194–6.
- Rosenn B, Miodovnik M, Dignan PS, et al. Minor congenital malformation in infants of insulin-dependent diabetic women: association with poor glycemic control. Obstet Gynecol 1990;76:745–9.
- Allen T, Thomson WM, Emmerton LM, Poulton R. Nutritional supplement use among 26-year-olds. N Z Med J 2000;113(1113):274–7.
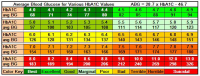
For example, if I calculate my mean BG from my meassured HbA1c, it should have been 99 mg/dl.
Actually measured it was 117! And from that meassured BG my calculated average HbA1c should have 5.7%.
My stack is described here.
I am currently taking different supplements one by one to see if they have any effect.
In my experience mainly diet helped me not to proceed from prediabetes. Supplements and drugs are a smaller contributing factor.
Edited by pamojja, 10 December 2017 - 12:35 PM.