Are there any alternatives to a telomere test?
Telomere tests aren't widely available, especially since Covid-19, and even when they were, had numerous issues.
I had a look for any correlations between leukocyte telomere length (LTL) and other blood markers.
Two stood out: C-reactive protein and neutrophil: lymphocyte ratio (known as NLR).
According to this recent paper, patients admitted to hospital with Covid-19 had significantly shorter telomeres than age matched controls.
Short telomeres increase the risk of severe COVID-19
We found a significantly higher proportion of patients with short telomeres (<10th percentile) in the COVID-19 patients as compared to the reference cohort (P<0.001). Short telomeres were associated with a higher risk of critical disease, defined as admission to intensive care unit (ICU) or death without ICU. TL was negatively correlated with C-reactive protein and neutrophil-to-lymphocyte ratio. Finally, lung tissue from patients with very short telomeres exhibit signs of senescence in structural and immune cells. Our results suggest that TL influences the severity of the disease.
https://www.aging-us...cle/104097/text
Note the reference made to the correlation between telomere length and C-reactive protein and NLR. In both cases the correlation was about -0.25. Another paper independently discovered the importance of NLR in Covid severity.
Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage
We found that NLR is a predictive factor for early-stage prediction of patients infected with COVID-19 who are likely to develop critical illness. Patients aged ≥ 50 and having an NLR ≥ 3.13 are predicted to develop critical illness, and they should thus have rapid access to an intensive care unit if necessary.
https://translationa...967-020-02374-0
Interestingly, this recent study into extremely long lived fish identified NRL as an important biomarker related to immune function that did not decline with age, and that was also correlated with LTL at -0.27, agreeing with the previous study.
No evidence of physiological declines with age in an extremely long‑lived fish
In this study we examined the potential relationship between age and multiple physiological systems including: stress levels, immune function, and telomere length in individuals ranging in age from 2 to 99 years old in bigmouth bufalo (Ictiobus cyprinellus), the oldest known freshwater teleost fish. Contrary to expectation, we did not find any evidence for age-related declines in these physiological systems. Instead, older fsh appeared to be less stressed and had greater immunity than younger fish, suggesting age-related improvements rather than declines in these systems.
https://doi.org/10.1...598-021-88626-5
This suggests immune function is essential to long life, even non-aging life, and it is closely related to telomere length in these cells, which may reflect a constant supply of progenitor cell replacements.
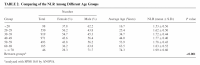
Rather like TL, NLR is an unreliable measure of aging but a robust indicator for health. For example in the following paper, NLR correlates only 0.16 with age but the average in each age category declines unequivocally, as can been seen in Table 2 (attached).
Neutrophil-to-Lymphocyte Ratio Positively Correlates to Age in Healthy Population
The eldest age group possessed the highest NLR and the youngest age group had the lowest NLR. NLR was also slightly positively associated with systolic pressure, diastolic pressure, and BMI (P < 0.001)
DOI 10.1002/jcla.21791
We can conclude that NLR varies widely for a given age, but declines reliably over a lifetime (sound familiar, anyone?).
The following paper backs up what we saw in the Covid-19 studies, indicating NLR is associated with all-cause mortality.
The neutrophil-to-lymphocyte ratio is associated with mortality in the general population: The Rotterdam Study
Inflammation is a risk factor for morbidity and mortality in the elderly. The neutrophil-to-lymphocyte ratio (NLR) is a marker of systemic inflammation that integrates the information of the leukocyte differentials into one variable. We aimed to assess whether the NLR is a risk indicator for overall and cause-specific mortality in the general population. …. The NLR was higher in men, higher age categories, smokers and among individuals with lower SES, prevalent diabetes, or a history of cancer or CVD. During the 11.7 years follow-up period, 1641 individuals died. Survival among individuals in the 3rd, 4th, and 5th quintile of the NLR was significantly poorer than that of those in the 1st quintile (P < 0.001). In the multivariable analysis, NLR levels were independently and significantly associated with an increased risk of all-cause mortality (HR 1.64; 95% CI 1.44–1.86), cardiovascular mortality (HR 1.92; 95% CI 1.49–2.48), and other mortality (HR 1.86; 95% CI 1.54–2.24). No significant association was found for cancer mortality (HR 1.20; 95% CI 0.95–1.51). The NLR is a strong and independent risk indicator for mortality in the elderly population
https://link.springe...0654-018-0472-y
In many ways C-reactive protein and NLR are interchangeable, with CRP being a somewhat less useful marker, which nevertheless moves in the same direction with age and ill health.
The baseline levels and risk factors for high-sensitive C-reactive protein in Chinese healthy population
Baseline levels of serum hs-CRP are increased with ageing and are significantly higher in male than female healthy population. In addition, elevated serum levels of hs-CRP are also associated with increased SUA but decreased HDL-c and SOD. Thus, serum levels of hs-CRP may be an indicator associated with ageing in healthy Chinese population.
The multivariate linear regression analysis further identified significant correlations between hs-CRP and age (β = 0.033, P = 0.012), the levels of HDL-c (β = − 0.062, P < 0.001), SOD (β = − 0.100, P < 0.001) and SUA (β = 0.033, P = 0.015).
https://immunityagei...2979-018-0126-7
At this point I have more than an inkling that measures of inflammation like CRP and measures of immune function like NLR and lymphocyte % are different facets of a more fundamental aging factor.
Conclusions
NLR and CRP are correlated with LTL and in the absence of a telomere test may serve as a useful proxy. At a deeper level, NLR and CRP are indicators of a root cause of chronic inflammation and immune dysfunction, which may be a consequence of telomere shortening and hence the underlying aging process.