The problems are only seen, as far as I can tell, in people who already have liver disease. In my opinion, at this moment at least, it is like saying that Potassium is dangerous because it can kill people with advanced renal disease.

Posted 22 May 2019 - 10:29 AM
The problems are only seen, as far as I can tell, in people who already have liver disease. In my opinion, at this moment at least, it is like saying that Potassium is dangerous because it can kill people with advanced renal disease.
Posted 22 May 2019 - 10:32 AM
I'm not sure if you are intentionally mis-reprensenting the literature or are not well versed in statistics. The study you cite has no statistical power:
151 liver-treatment patients filled out a questionaire, 23 took glucosamine, the authors claim, that from the records they could causally attribute 2 cases of altered liver encymes to glucosamine (though not attributing any functional changes or actual toxicity to glucosamine).
This is not even a prospective cohort study. It's just a questionaire of 151 people. They don't even attempt to calculate confounding factors for the 151 people - different drugs etc. and their relations - just noting in these 2 case studies, that there is a coincidence with glucosamine and no common liver damaging behaviour. Albeit for one of the 2 cases they even acknowledge that it turned out to be a case of hepatitis.
Are you seriously claiming that this article gives any scientific clue about side effects? If yes we first would need a discussion about different kinds of evidence in bioscience and the use of statistics. Anecdotal evidence as in this study is of very limited use.
As outlined in the glucosamine and cancer thread:
there are very well controlled for, prospective cohort studies, with 10th of thousands of participants. Those have good statistical power, delivering highly statistical significant results AFTER accounting for dozens of confounding factors. In addition the reduction in relative risk calculated for total mortality and cancer (for users of glucosamine vs. non-users) is not small, but huge. That's still not a scientific proof for a causal relationship! But at least it's not just anecdotal evidence.
If you are looking for a comprehensive scientific study of side effects you could start here:
https://mafiadoc.com...bc5223bd8f.html
An analysis of many RCTs (randomized, placebo controlled trials) of glucosamine in people showed no toxic effects for a broad spectrum of organs and blood values. Feeding animals truely stupendous amounts of glucosamine for up to 1 year did not result in any alterations in liver tissue (or other side effects for that matter). For a different series of RCTs in people that compare subjective reports of side effects compared to placebo and NSAID, the authors even note:
"In 13 of the 18 studies, symptoms were reported less commonly in glucosamine-treated subjects than in placebo-treated subjects;"
Yes, you are reading this correctly: glucosamine has less reported side-effects than placebo.
They tried to find studies for LD50 in animals (the dosis, that kills half of the study subjects). They did not succeed, as even force feeding and injecting mice with mega dosis of glucosamine did not result in any toxicity. As we know from the 2014 mice-lifespan study they just live longer and healthier.
3 grams of glucosamine is "too much" - based on what? It's dirt cheap over the internet; it's well below the only side effect reported in humans: a headache in 1 of 10 volunteers after being intravenously injected with 30 gram of glucosamine at once. It's MUCH safer than metformin. If you truly worry about side effects of glucosamine you should consequently stop metformin and arguably most other stuff you are taking.
Edited by Guest, 22 May 2019 - 10:37 AM.
Posted 22 May 2019 - 08:53 PM
To offer more food for thought, another comment to bio-availability:
there are 2 studies done for bio-availability of Glucosamine (GS) in humans; the more important one being:
"Glucosamine oral bioavailability and plasma pharmacokinetics after increasing doses of crystalline glucosamine sulfate in man": https://www.oarsijou...0193-7/fulltext
Their main findings:
- GS got an elimination half-life of about 15 hours in humans
- an oral doses up to 1,5 gram in on sitting is readily absorbed and increases plasma concentration of GS proportionally compared to 0,75 gram
- oral intake of 3 gram of GS in one sitting did result in a less than proportional increase in plasma levels
This indicates, that you might want to spread out taking a GS intake of 3 gram or more per day - i.e. a little in the morning and a little in the evening - to get the most out of it.
To make you scratch your head a little more, let's have a look at the actual GS-uptake mechanism. This picture illustrates the structure of glucosamine to the left and glucose to the right. Both are simple molecules - the only difference being the exchange of on hydroxy-group by one amino-group:

Glucosamine in principle utilities the same cellular transporters as glucose. But there is one strange difference: GLUT2 - a glucose transporter that is especially prevalent in the nutrient absorbing small intestines and does not require insulin to be activated - is highly sensitive to glucosamine:
"GLUT2 is a high affinity glucosamine transporter"
https://www.scienced...014579302030582
According to above study this glucose transporter actually is 21-fold as sensitive to glucosamine as it is for glucose itself - meaning glucose requires a 21-fold concentration in the medium to be transported at the same rate as is glucosamine. The liver got an elevated concentration for GLUT2 as well. This combination could be the explanation for the good bio-availability of oral glucosamine in blood plasma.
As mentioned before, in one mice study, administering the human equivalent of 3 gram glucosamine per day resulted in more active autophagy than caloric restriction. The results looked like this:
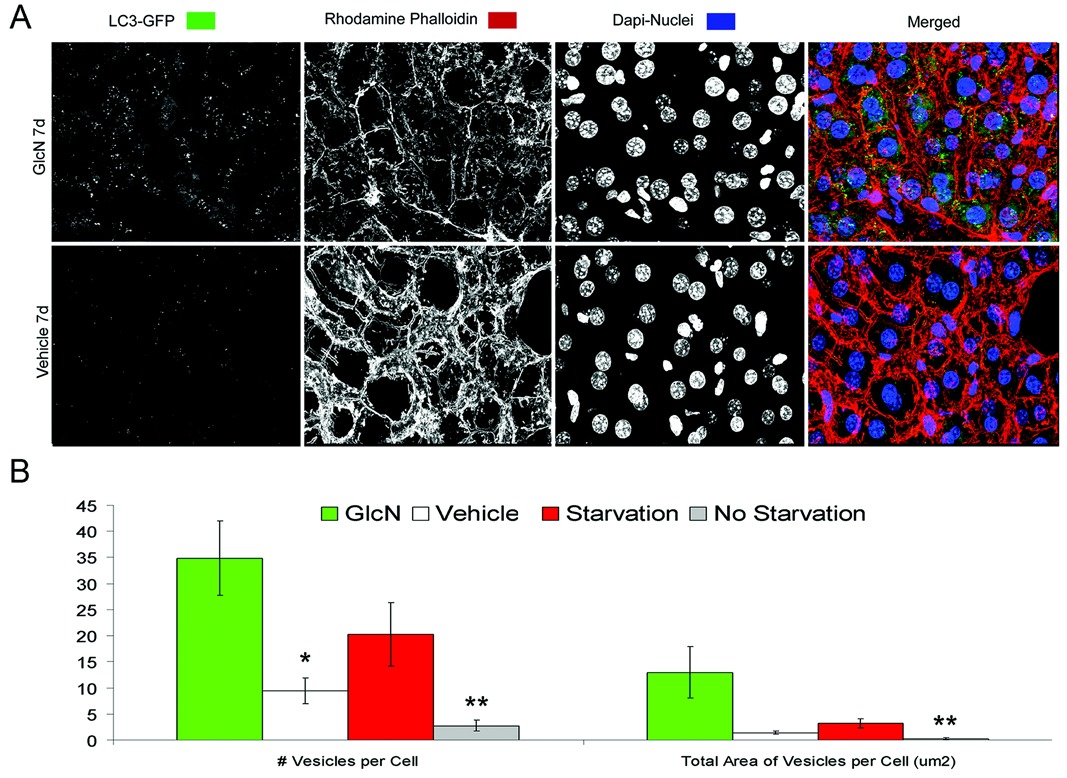
yellow - glucosamine
white - controls
red - caloric restriction
grey - a different mouse strain as further controls
Although GS and glucose are structurally almost identical, the effects are very markedly different. The controls got glucose as part of their lab diet (as did the treatment groups). Starving the mice on a water-only fast (and consequently no glucose) did increase AP. But using a rather small dose of GS in addition to a normal glucose intake resulted in a considerably stronger AP.
It appears, that GS got an effect on AP that goes beyond competing against glucose. So it could be more to GS than just mimicking a reduced carb diet.
Glucosamine:
- much safer than metformin
- better life extension effects in mice than metformin
- life-extension in a prospective cohort study in healthy humans - 22% reduced all-cause mortality rate in on analysis of the VITAL-data (or even up to 49% reduced all-cause mortality rate if you believe the analysis of only the participants that did no use NSAID... but I personally think that's just a statistical fluke)
- and the cancer-studies concluded, that there is a dose-depended effect - the more you take, the better the benefits... and GS is very safe
- potentially better AP than caloric restriction using a rather small dose...
Give me a reason, why anyone is taking metformin for purely life-extension purposes - but not glucosamine. Or Vitamin K2 (it's got less evidence than GS going for it). Or a dozend other less impressive supplements, that even deliver less impressive safety-records.
Edited by Guest, 22 May 2019 - 09:07 PM.
Posted 22 May 2019 - 10:25 PM
When I read this thread I got some of the glucosamine I had from the bottle and consumed it. It's pretty salty.
Chondroitin had some extension benefits too right? When I take glucosamine I don't notice any benefit to my joints.
The stuff I had is sulfate.
Posted 22 May 2019 - 10:30 PM
Interesting that he might still be taking Glucosamine. I wonder if the warning which he included in his discussion is not applicable at the doses he/we might take it at? Maybe it should be cycled?
There may be a downside to taking too much glucosamine
A 2010 publication suggests that taking high doses of glucosamine or prolonged use it glucosamine reduces levels of SIRT1, leads to apoptosis of pancreatic cells and could increase the risk of developing diabetes. Hexosamines stimulate apoptosis by altering T1 action and levels in rodent pancreatic β-cells: “The activity and levels of SIRT1, which promotes cell survival in several models, are linked to glucose concentrations and cellular energy metabolism. The present study aimed to determine whether impaired Sirt1 activity is involved in the induction of apoptosis by the nutrient-sensing hexosamine biosynthesis pathway (HBP). Pancreatic Nit-1, Rin-m5F, and Min6 β-cells were acutely treated at different doses and times with glucosamine, which enters and stimulates the HBP. Sirt1 levels were genetically modulated by retroviral infection. Expression levels, cellular localization, and activity of apoptosis-related markers were determined by qPCR, immunoblotting, and co-immunoprecipitation. Glucosamine treatment dose- and time dependently induced cell apoptosis in all cell lines studied. HBP stimulation time dependently modified SIRT1 protein levels, notably in the cytoplasm. This was concomitant with increased E2F1 binding to the c-myc promoter. In both NIT-1 and min6 β-cells, genetic knockdown of Sirt1 expression resulted in higher susceptibility to HBP-stimulated apoptosis, whereas overexpression of Sirt1 had the opposite impact. These findings indicate that reduction of SIRT1 levels by hexosamines contributes to β-cell apoptosis. Methods to increase SIRT1 levels or activity could thus prevent the decrease in β-cell mass, notably that observed in type 2 diabetes.”
Relative to this issue, the 2014 publication 17A-Estradiol protects against glucosamine-induced pancreatic A-cell dysfunction concludes “: GlcN impairs insulin secretion of [beta]-cells by inhibiting Ca2+ influx and enhancing [beta]-cell apoptosis with increases in ER stress-related proteins, whereas E2 counters these adverse effects of GlcN.”
Posted 22 May 2019 - 10:49 PM
Their main findings:
- GS got an elimination half-life of about 15 hours in humans
- an oral doses up to 1,5 gram in on sitting is readily absorbed and increases plasma concentration of GS proportionally compared to 0,75 gram
- oral intake of 3 gram of GS in one sitting did result in a less than proportional increase in plasma levels
This indicates, that you might want to spread out taking a GS intake of 3 gram or more per day - i.e. a little in the morning and a little in the evening - to get the most out of it.
Thanks, I have been doing 4 grams at once, but based on this I will now do 2 grams in am and 2 in pm, excellent research here.
Posted 22 May 2019 - 10:55 PM
I don't get it...
Are people in this forum really so scientifically illiterate? I'm slowly starting to get the impression as if nothing I'm explaining is getting through.
The study you are citing is an in-vitro study! You are looking at cells and cells cultures in a petri dish. That is not necessarily how the substances is affecting the tissue in a living organism, where numerous metabolic tissue responses are active and metabolic feedback-loops that interact with other organs and hormones. In-vitro can be useful to understand the mechanism behind an established in-vivo (meaning in a living organism) effect.
And we already have plenty of in-vivo data in animals and humans - manifesting itself as numerous extensive RCTs for side effects including effects on glucose metabolism and pancreatic tissue. The very study I was alluding in my posts about no side-effects has an entire section about potential effects on glucose regulation. There are none. As is supported by more recent analysis of in-vivo data:
"A comprehensive review of oral glucosamine use and effects on glucose metabolism in normal and diabetic individuals"
https://www.ncbi.nlm...les/PMC3042150/
There are extensive cohort studies in living humans that demonstrate substantial long-term benefits. And a life-extension study in mice demonstrating substantial effects in already old mice.
Please folks:
it's good to be sceptical. But use common sense. If you want to disprove dozends of RCTs and extensive prospective cohort studies DO NOT use anecdotal evidence and in-vitro studies. Use RCTs or cohort studies that demonstrate negative effects. In-vitro data or anecdotal data alone is almost useless.
Edited by Guest, 22 May 2019 - 11:03 PM.
Posted 23 May 2019 - 04:13 AM
When I read this thread I got some of the glucosamine I had from the bottle and consumed it. It's pretty salty.
Chondroitin had some extension benefits too right? When I take glucosamine I don't notice any benefit to my joints.
The stuff I had is sulfate.
I would stay far away from chondroiton.
Use of glucosamine and chondroitin supplements in relation to risk of colorectal cancer: Results from the Nurses' Health Study and Health Professionals follow-up study.
Kantor ED, et al. Int J Cancer. 2016.AbstractRecent epidemiologic evidence has emerged to suggest that use of glucosamine and chondroitin supplements may be associated with reduced risk of colorectal cancer (CRC). We therefore evaluated the association between use of these non-vitamin, non-mineral supplements and risk of CRC in two prospective cohorts, the Nurses' Health Study and Health Professionals Follow-up Study. Regular use of glucosamine and chondroitin was first assessed in 2002 and participants were followed until 2010, over which time 672 CRC cases occurred. Cox proportional hazards regression was used to estimate relative risks (RRs) within each cohort, and results were pooled using a random effects meta-analysis. Associations were comparable across cohorts, with a RR of 0.79 (95% CI: 0.63-1.00) observed for any use of glucosamine and a RR of 0.77 (95% CI: 0.59-1.01) observed for any use of chondroitin. Use of glucosamine in the absence of chondroitin was not associated with risk of CRC, whereas use of glucosamine + chondroitin was significantly associated with risk (RR: 0.77; 95% CI: 0.58-0.999). The association between use of glucosamine + chondroitin and risk of CRC did not change markedly when accounting for change in exposure status over follow-up (RR: 0.75; 95% CI: 0.58-0.96), nor did the association significantly vary by sex, aspirin use, body mass index, or physical activity. The association was comparable for cancers of the colon and rectum. Results support a protective association between use of glucosamine and chondroitin and risk of CRC. Further study is needed to better understand the chemopreventive potential of these supplements.
Glucosamine alone - no problems. Add in chondroiton - colorectal cancer rates rise.
Posted 23 May 2019 - 07:15 AM
btw i wasnt picking on glucosamine. for the people who are attacking me for posting the study relation to liver disease, im just trying to be informative of whats out there. its strange that regardless of how good glucosamine is, that none of the supporters of it ever post anything negative even if inconclusive. at least try to be open mind, informative as much as possible. post something positive but try to look the other way too please. there are probably many more studies showing side effects but supporters wont post them. and i would not dare either, because im being picked on by doing so. you guys do as you please and i apologize for checking side effect profile through google
Edited by GABAergic, 23 May 2019 - 07:16 AM.
Posted 23 May 2019 - 11:24 AM
Very interesting study, thanks for that. I'll read it thoroughly ASAP but in order to know whether GS is simply a carb restriction mimetic or more, we'd need to know when the calorie restriction mice were fed and when autophagy was measured. Even on calorie restriction if food is available 24hrs a day then autophagy will be downregulated whenever insulin or mTOR is activated.It appears, that GS got an effect on AP that goes beyond competing against glucose. So it could be more to GS than just mimicking a reduced carb diet.
Edited by QuestforLife, 23 May 2019 - 11:47 AM.
Posted 23 May 2019 - 12:16 PM
I would stay far away from chondroiton.
Glucosamine alone - no problems. Add in chondroiton - colorectal cancer rates rise.
Posted 23 May 2019 - 01:42 PM
Use of glucosamine + chondroitin was significantly associated with risk (RR: 0.77; 95% CI: 0.58-0.999) Isn't that risk significantly reduced, though? I asume that normal RR is 1, and there is 0.77.
That's always how I understood Risk Ratio.
From Wikipedia:
Risk ratio is used in the statistical analysis of the data of experimental, cohort and cross-sectional studies, to estimate the strength of the association between treatments or risk factors, and outcome.%5B2%5D%5B3%5D For example, it is used to compare the risk of an adverse outcome when receiving a medical treatment versus no treatment (or placebo), or when exposed to an environmental risk factor versus not exposed.
Assuming the causal effect between the exposure and the outcome, values of RR can be interpreted as follows:
Posted 23 May 2019 - 01:56 PM
Use of glucosamine + chondroitin was significantly associated with risk (RR: 0.77; 95% CI: 0.58-0.999) Isn't that risk significantly reduced, though? I asume that normal RR is 1, and there is 0.77.
Yeah sorry its worded poorly and I got confused. It says
Use of glucosamine in the absence of chondroitin was not associated with risk of CRC, whereas use of glucosamine + chondroitin was significantly associated with risk (RR: 0.77; 95% CI: 0.58-0.999).
which sounds like chondroiton is positvely associated with cancer risk, but then it concludes by saying
Results support a protective association between use of glucosamine and chondroitin and risk of CRC. Further study is needed to better understand the chemopreventive potential of these supplements.
So its protective. My bad. I was wrong.
Posted 23 May 2019 - 02:04 PM
Yeah sorry its worded poorly and I got confused. It says
which sounds like chondroiton is positvely associated with cancer risk, but then it concludes by saying
So its protective. My bad. I was wrong.
Posted 23 May 2019 - 02:04 PM
It's not your wording that is the problem, it is the study's.
Use of glucosamine in the absence of chondroitin was not associated with risk of CRC, whereas use of glucosamine + chondroitin was significantly associated with risk (RR: 0.77; 95% CI: 0.58-0.999).
They are saying glucosamine + chondroitin has a risk ratio of 0.77 for colorectal cancer. That tells me that the exposure group (glucosamine + chondroitin) had a lower incidence of CRC than the unexposed group. Either that is a misprint or I have to really question the knowledge of the people that wrote this paper. Unless I just don't understand the definition of risk ratio.
Posted 23 May 2019 - 02:59 PM
Very interesting study, thanks for that. I'll read it thoroughly ASAP but in order to know whether GS is simply a carb restriction mimetic or more, we'd need to know when the calorie restriction mice were fed and when autophagy was measured. Even on calorie restriction if food is available 24hrs a day then autophagy will be downregulated whenever insulin or mTOR is activated.
The authors of that mice-paper used a somewhat imprecise language throughout the paper - but there is a sentence, that mentions that the mice got a 48-hour water-only fast and got sacrificed at that point. Unrestricted access to water. No food.
The intervention group got a normal lab diet + Glucosamine for 7 days and killed at that point.
So in human terms it's more a comparison of AP after a week-long fast vs. chronic Glucosamine exposure in people eating normally. Glucosamine got the stronger AP. A strong AP-response upon Glucosamine exposure (5 days after megadosis infusion) was observed in 1972 as well, in the study that treated cancer-rats using Glucosamine.
Posted 23 May 2019 - 03:00 PM
This very recent study is not about autophagy or about CRC but gives an indication of the safety and effectiveness of supplementing GS. 466.000 healthy people were followed over a number of years. The GS users had significantly less CVD incidence:
https://www.ncbi.nlm...pubmed/31088786
Posted 23 May 2019 - 03:34 PM
I wonder what paper does chondroitin play in all of this, I take both at the time.
Posted 23 May 2019 - 05:01 PM
It's not your wording that is the problem, it is the study's.
They are saying glucosamine + chondroitin has a risk ratio of 0.77 for colorectal cancer. That tells me that the exposure group (glucosamine + chondroitin) had a lower incidence of CRC than the unexposed group. Either that is a misprint or I have to really question the knowledge of the people that wrote this paper. Unless I just don't understand the definition of risk ratio.
I used to just read the abstracts, and rely upon popular media reports about studies (takes too much time to read through a lot of papers). When I do read through medical research, I am amazed at how confusing a lot of it is. Some have poor grammar. Some have statistical errors. We have a thread here at LongeCity about problems in medical research, most of which arises from in-vitro or animal research. I once used the term "junk science" which might be a little harsh, but it needs to improve.
Posted 23 May 2019 - 05:39 PM
The authors of that mice-paper used a somewhat imprecise language throughout the paper - but there is a sentence, that mentions that the mice got a 48-hour water-only fast and got sacrificed at that point. Unrestricted access to water. No food.
The intervention group got a normal lab diet + Glucosamine for 7 days and killed at that point.
So in human terms it's more a comparison of AP after a week-long fast vs. chronic Glucosamine exposure in people eating normally. Glucosamine got the stronger AP. A strong AP-response upon Glucosamine exposure (5 days after megadosis infusion) was observed in 1972 as well, in the study that treated cancer-rats using Glucosamine.
Posted 23 May 2019 - 06:56 PM
Injecting a substance will of course lead to a higher blood level than oral ingestion.
As GS seems to be a very benign compound (compared to Metformin and especially Rapamycin) - and the cancer studies indeed indicate a dose-response-relationship - it might be sufficient to just up the amount taken. If absorption levels off, if taken at 3 grams or more at once, it should still be possible to take it 1 or 2 hours apart. The powdered version of GS might be better for that purpose, as you can sprinkle it into drinks or on food.
As for anabolism/catabolism and AP for longevity I'm not so certain. The mice in the GS-lifespan-study received GS as part of their diet, i.e. mixed into their normal lab food. It's similarly done in the Rapamycin lifespan-studies. Maybe intermittent administration could lead to better outcomes. Is there any animal data available for that?
Posted 23 May 2019 - 07:19 PM
Posted 23 May 2019 - 07:35 PM
also i still cant figure out what form of glucosamine is the one studied with positive effects. and which is associated with more side effects. as if the studies werent confusing enough. personally i believe in NAG, n-acetyl glucosamine but is this form even involved in any studies?
Edited by GABAergic, 23 May 2019 - 07:35 PM.
Posted 24 May 2019 - 04:14 AM
Studies use either Glucosamine sulfate or Glucosamine hydrochloride. NAG behaves biochemically very different than Glucosamine and is not used in any of those studies. The HCl-version of GS is more commonly used in animal studies on cancer and AP, the sulfate version commonly used in human studies and is the most prevalent as a supplement (and consequently in the cancer studies in humans). Both should be fine.
Another data point for GS:
"Glucosamine improves survival in a mouse model of sepsis and attenuates sepsis-induced lung injury and inflammation. (2019)"
http://www.jbc.org/c.../294/2/608.long
"To examine the effects of GlcN on septic mortality, we monitored mouse survival after cecal ligation and puncture (CLP) with or without GlcN (200 mg/kg) for 12 days (Fig. 1A). Based on Kaplan-Meier survival curves, mice with CLP-induced sepsis presented a 12-day survival rate of 11%. GlcN pretreatment increased the 12-day survival rate to 55% relative to that in mice with untreated sepsis (Fig. 1B). All sham-operated control mice treated with or without GlcN survived."
Albeit this study is a little strange:
- they say, that each group got n = 10 mice; that should make 11% or 55% results impossible... it maybe just a typo
- GS is anti-inflammatory; so why does it seem to aid fighting off infections? If anything I would have expected that it downregulates immunity, as is sometimes discussed for caloric restriction.
Posted 24 May 2019 - 06:33 AM
Posted 24 May 2019 - 11:19 AM
I have two things to add:
1) I remember Valter Longo saying in a Rhonda Patrick interview that he don't want to use Metformin, because he dislike the idea of inhibiting such an important pathway as mTOR. In his words, mTOR is highly important and he adds to idea of alteranting cycles like fasting and refeeding. So I think that autophagy and a times of anabolism are important.
The reason why fasting works for autoimmune conditions is because fasting eliminates damaged and old immune cells and then replaces it with new ones after refeeding. If I remember well, Rapamycin works in a similar way, it inhibits anabolic pathways, and the damaged cells could be cleared by autophagy.
Posted 24 May 2019 - 11:29 AM
2) A potential use of Glucosamine for boosting autophagy/ reducing the time needed for enter into ketosis.
Fasting starts to feel well by the third day, in that day ketone bodies are at full. However one of the problems with fasting is that you need to stay 5 days in the FASTING MIMICKING DIET and you need to wait to the third to start to feel great, so there is a way of reducing the time needed for enter into full ketosis?. As we know ketosis and autophagy go hand in hand
Niacin+Glucosamine at night.
Perhaps this is the best way of boosting autophagy, taking Niacin before going to sleep+Glucosamine. Autophagy works better at night while sleeping, and Niacin apparently could produce an state of ketosis it flushes glucose from the liver and blocks FFA release, followed by a rebound of FFA after an hour. Niacin increases HGH also. Fasting does similar things and there are studies showing that lower insulin levels are correlated with increased HGH.
In my experiments with Niacin, it makes me sleep like a baby, I sleep less hours and wake up in a better mood. If I sleep too much after taking Niacin then I start to feel drowsy with low energy, I just want to sleep more, so apparently after some hours Niacin makes me hypoglicemic
What do you think about this?
Edited by BieraK, 24 May 2019 - 11:31 AM.
Posted 24 May 2019 - 11:38 AM
As I understand it, autophagy is something that needs time to become operational. So a 12 hour fast would not make it kick-in. Similarly if you don't allow an AP-causing stimulus sufficient time to run it's course, you would not get a good AP-response.
Caloric restriction is a chronic stimulant of AP. If you do CR for a day, then a day of normal eating, again a day on CR etc. - you would not get good AP. The reason might be, that CR (as done in humans) is just not a strong AP-inducer and thus needs more time to fully establish the effect.
Rapamycin as a pharmacologic agent appears to be able to strongly activate AP, therefore a short exposure of a couple of hours induces considerable AP.
Glucosamine is a less potent total AP-inducer gram for gram. So if you take 1,5 gram of GS once daily I find it questionable to get the strong AP-response seen in the mice-study. Maybe taking 3-6 gram spread over 1-2 hours is strategy to kick-start AP and still have the effect vanish after 24 hours. About 6 gram per day was the human equivalent amount (by the most common method of allometric scaling) used in the mice-lifespan-study. But it was part of the food and eaten spread out over a day, i.e. chronic exposure as in caloric restriction.
Posted 24 May 2019 - 05:49 PM
We're about off topic but as it's relevant to your question I'll share some of my personal regime. I fast 16-18 hours per day (basically have dinner early and miss breakfast). I've found this to be remarkably potentiated by a strong coffee in the morning first thing, and a decaffeinated coffee last thing before bed.2) A potential use of Glucosamine for boosting autophagy/ reducing the time needed for enter into ketosis.
Fasting starts to feel well by the third day, in that day ketone bodies are at full. However one of the problems with fasting is that you need to stay 5 days in the FASTING MIMICKING DIET and you need to wait to the third to start to feel great, so there is a way of reducing the time needed for enter into full ketosis?. As we know ketosis and autophagy go hand in hand
Niacin+Glucosamine at night.
Perhaps this is the best way of boosting autophagy, taking Niacin before going to sleep+Glucosamine. Autophagy works better at night while sleeping, and Niacin apparently could produce an state of ketosis it flushes glucose from the liver and blocks FFA release, followed by a rebound of FFA after an hour. Niacin increases HGH also. Fasting does similar things and there are studies showing that lower insulin levels are correlated with increased HGH.
In my experiments with Niacin, it makes me sleep like a baby, I sleep less hours and wake up in a better mood. If I sleep too much after taking Niacin then I start to feel drowsy with low energy, I just want to sleep more, so apparently after some hours Niacin makes me hypoglicemic
What do you think about this?
Edited by QuestforLife, 24 May 2019 - 05:52 PM.
Posted 24 May 2019 - 07:34 PM
That's curious. I wasn't aware of the coffee-mortality literature. However, I'm not so sure that Coffee and Glucosamine employ the same mechanisms. According to this cohort study:
Association of Coffee Consumption With Overall and Cause-Specific Mortality in a Large US Prospective Cohort Study (2015)
https://www.ncbi.nlm...les/PMC5875735/
coffee is associated with reduced risk for CVD and respiratory illnesses - but not cancer.
Glucosamine also is associated with reduced CVD risk and respiratory illnesses - but most remarkably it's got a strong anti-cancer effect. It's not entirely clear by what mechanism this effect occurs (speculation is about anti-inflammatory effects, effects on mitochondrial respiration and glucose metabolism), so it might not be directly related to autopagy.
0 members, 30 guests, 0 anonymous users