.
F U L L T E X T S O U R C E : BiorRXiv
Abstract
While many diseases of aging have been linked to the immunological system, immune metrics with which to identify the most at-risk individuals are lacking. Here, we studied the blood immunome of 1001 individuals age 8-96 and derived an inflammatory clock of aging (iAge), which tracked with multi-morbidity and immunosenescence. In centenarians, iAge was on average, 40 years lower than their corresponding chronological age. The strongest contributor to this metric was the chemokine CXCL9, which was involved in cardiac aging, affected vascular function, and down-regulated Sirtuin-3, a longevity-associated molecule. Thus, our results identify an important link between inflammatory molecules and pathways known to govern lifespan.
Introduction
The role of the immune system in the maintenance of human health and protection against infections has been recognized for over a hundred years. However, it was only in the past few decades that it has become apparent that inflammatory components of the immune system are often chronically elevated in aged individuals and associated with an increased incidence of cancer, cardiovascular disease and neurodegenerative disorders, among others (Crusz and Balkwill, 2015; Kotas and Medzhitov, 2015; Liu et al., 2017). From these observations, it has been postulated that inflammation plays a critical role in regulating physiological aging (Franceschi and Campisi, 2014; Furman et al., 2017b). Furthermore, the well-established nine hallmarks of aging (Lopez-Otin et al., 2013); (1) genomic instability, (2) shortening telomere length, (3) epigenetic modifications, (4) loss of proteostasis, (5) deregulated nutrient sensing, (6) mitochondrial dysfunction, (7) cellular senescence, (8) stem cell exhaustion, and (9) altered intracellular communication, have all been shown to be caused, at least in part, by sustained systemic inflammation (Cavadas et al., 2016; Efeyan et al., 2015; Grivennikov et al., 2010; Hunter et al., 2007; Jurk et al., 2014; Lasry and Ben-Neriah, 2015; Nathan and Cunningham-Bussel, 2013; Oh et al., 2014; Thevaranjan et al., 2017; Alpert et al., 2019).
Contrary to the acute response, which is typically triggered by infection, chronic and systemic inflammation is thought to be triggered by physical, chemical or metabolic noxious stimuli (“sterile” agents) such as those released by damaged cells and environmental insults, generally termed “damage-associated molecular patterns” (DAMPs). This type of inflammation is associated with aging and characterized by being low-grade and persistent, ultimately leading to collateral damage to tissues and organs (Goldberg and Dixit, 2015; Kotas and Medzhitov, 2015). Despite the importance of this type of inflammatory reaction, there are currently no standard biomarkers to define a chronic inflammatory state and studies have generally yielded conflicting results (Franceschi et al., 2017; Morrisette-Thomas et al., 2014).
To better define biological markers of chronic inflammation and disease, we set out to establish a broad survey of immunity in over 1000 individuals (the Stanford 1000 Immunomes Project or Stanford 1KIP), wherein biological samples from 1001 subjects were obtained in the years 2007-2016 and comprehensively measured in a single facility; the Stanford Human Immune Monitoring Center (HIMC). At this center peripheral blood specimens were processed and analyzed using multiple technological platforms such as serum cytokines, cell subset composition, the cellular responses to multiple stimuli and the seropositivity to cytomegalovirus infection. In 902 subjects, a comprehensive health assessment using a 53-feature clinical questionnaire was also obtained.
Given the well-established importance of chronic inflammation for many human diseases and the lack of standard measures of it, we used deep learning methods to construct a metric for age-related chronic inflammation (iAge), which correlated with multiple morbidities and markers of immunosenescence, and was significantly lower in centenarians. In a validation study of 97 healthy older adults who were also monitored at the HIMC (Stanford) for the same inflammatory markers, along with a 27-feature cardiovascular phenotyping screening at the Stanford Cardiovascular Institute, we found that the most robust contributor to iAge, the interferon-related chemokine CXCL9, tracked with subclinical cardiac remodeling and arterial stiffness. This chemokine was also expressed in large quantities by aged endothelium derived from human induced pluripotent stem cells (hiPSC), suppressed vascular function in mice aortic tissue, and inhibited expression of the cardio-protective longevity-associated deacetylase Sirtuin-3.
Thus, our results define healthy versus unhealthy aging and identify a link between inflammatory molecules of the immune system and known pathways governing lifespan in humans and in model organisms.
Results
Study design of the Stanford 1000 Immunomes Project
During the years 2007 to 2016, blood samples from ambulatory subjects (N = 1001) (339 males and 662 females) from age 8 to >89 (Fig. S1 and Fig. S2) who had been recruited at Stanford University (the Stanford 1000 Immunomes Project, or Stanford 1KIP) for a longitudinal study of aging and vaccination (Blazkova et al., 2017; Brodin et al., 2015; Furman et al., 2017b; Furman et al., 2014; Furman et al., 2013; Furman et al., 2015; Price et al., 2013; Roskin et al., 2015; Shen-Orr et al., 2016; Wang et al., 2014), and for an independent study of chronic fatigue syndrome (Montoya et al., 2017), from which only healthy controls were included. Inclusion and exclusion criteria can be found under the Methods section. For all samples of the Stanford 1KIP, deep immune phenotyping was conducted at the Stanford Human Immune Monitoring Center (HIMC), where peripheral blood specimens were processed and analyzed using rigorously standardized procedures (Maecker et al., 2012). Serum samples were obtained and used for protein content determination (including a total of 50 cytokines, chemokines and growth factors) (N = 1001) and to assess cytomegalovirus status (N = 748), a major determinant of immune system variation (Brodin et al., 2015; Furman et al., 2015). Peripheral blood mononuclear cells or whole blood samples were used for the determination of cellular phenotypes and frequencies (N = 935), and for investigation of in vitro cellular responses to a variety of cytokine stimulations (N = 818). Extended clinical report forms were collected from 902/1001 subjects, of which 299 were males and 603, females (Table S1 and S2). A total of 37 additional older adults (19 centenarians and 18 controls) were included and screened for serum protein content to derive iAge on these extremely long-lived humans.

Supplementary Figure 1
1000 Immunomes Study design: systematic analysis of immune systems via ‘OMICS’ approaches.
The Stanford 1000 Immunomes Project consist of 1001 ambulatory subjects age 8 to >89 (34% males, 66% females) recruited during the years 2007 to 2016 for a longitudinal study of aging and vaccination (Blazkova et al., 2017; Brodin et al., 2015; Furman et al., 2017; Furman et al., 2014; Furman et al., 2013; Furman et al., 2015; Price et al., 2013; Roskin et al., 2015; Shen-Orr et al., 2016; Wang et al., 2014), and for an independent study of chronic fatigue syndrome (Montoya et al., 2017) from which only healthy controls were included. For all samples of the Stanford 1KIP, deep immune phenotyping was conducted at the Stanford Human Immune Monitoring Center, where peripheral blood specimens were isolated and analyzed using standard procedures. Peripheral blood samples were obtained by venipuncture and peripheral blood mononuclear cells or whole blood samples were used for determination of cellular phenotypes and frequencies (N = 935) and for investigation of in vitro cellular responses to a variety of cytokine stimulations (N = 818); serum samples were obtained and used for protein content determination (including a total of 50 cytokines, chemokines and growth factors) (N = 1001). Clinical characterization was assessed via clinical questionnaire in a total of 902 subjects who completed the full set of 53 clinical items. From a total of 97 healthy young and older adults, comprehensive cardiovascular phenotyping was also conducted.
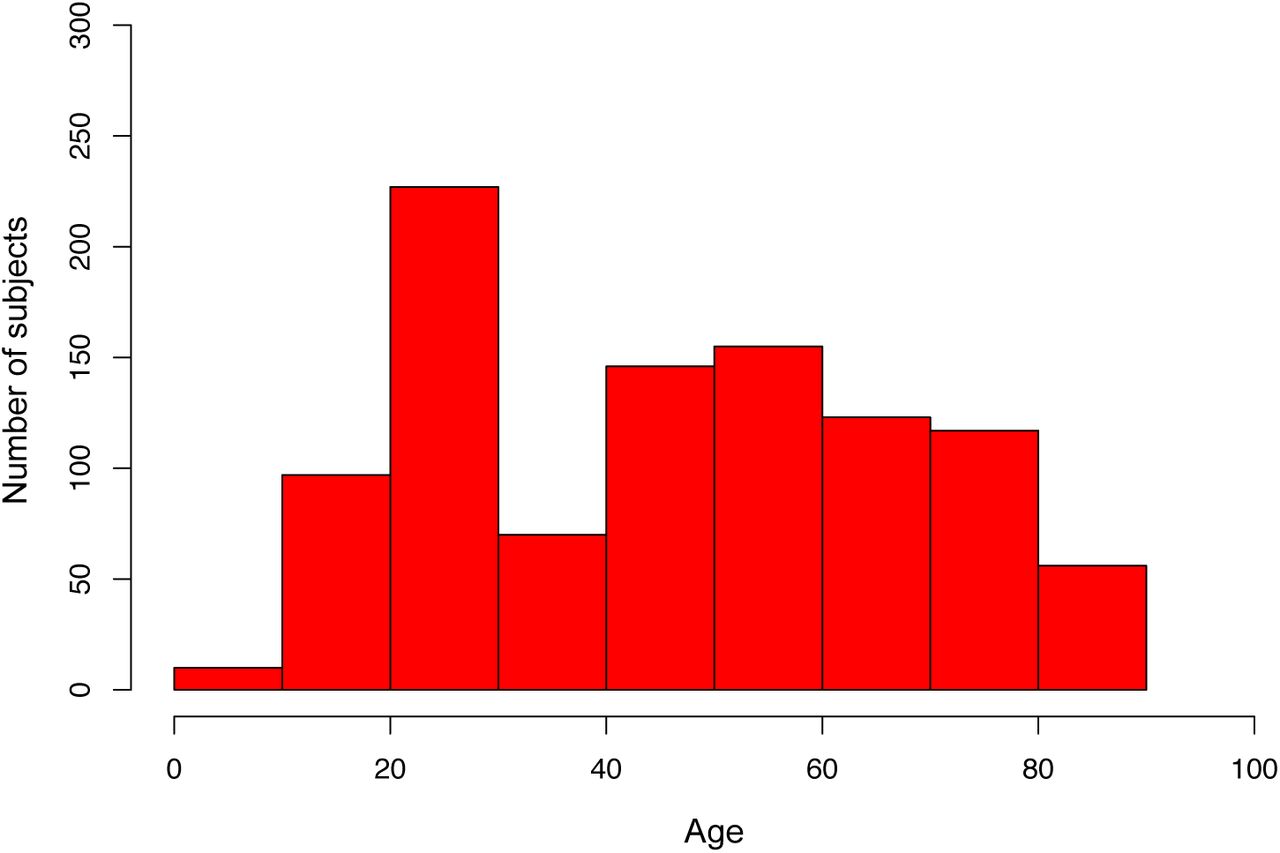
Supplementary Figure 2.
Age distribution of the Stanford 1KIP cohort.

Supplementary Table 1.
Available data for the 1000 Immunomes Project

Supplementary Table 2.
Number of subjects included, and analytical platform used for each study year.
Deep learning analysis of circulating immune cytokines and chemokines to derive a signature for age-related chronic inflammation
Given the increasingly recognized effect of low-grade systemic chronic inflammation in the development of a wide variety of diseases associated with aging, especially in cardiovascular disease (Furman et al., 2017b; Ridker et al., 2017), we set out to construct a metric for age-related chronic inflammation that could summarize an individual’s inflammatory burden. This type of inflammation is thought to ensue as a maladaptive reaction in response to exposure to tissue damage, metabolic dysfunction and environmental insults (collectively referred to as the “exposome”) (Goldberg and Dixit, 2015; Kotas and Medzhitov, 2015). In contrast to the acute inflammatory response, for which a number of secreted molecules (such as C-reactive protein, IL-1β, IL-6 and TNF-α) have been validated; in age-related chronic inflammation, no standard cytokine signature exists (Franceschi et al., 2017; Morrisette-Thomas et al., 2014). Thus, we undertook an unbiased approach to compactly represent the non-linear structure of the cytokine network. To do so, we used a deep learning method called guided auto-encoder (GAE) to circulating immune protein data encompassing a total of 50 cytokines, chemokines and growth factors from all 1001 subjects.
In the GAE method, the original data are combined in silico into a small number of ‘codes’ by a non-linear function. In this initial step, a first ‘hidden layer’ of a neural network is built. By combining each ‘code’ from the hidden layer into a new set of codes, iteratively, a second and third hidden layers are generated (for example, see Methods). This process aims at eliminating the noise and redundancy in the data, yet retaining the most relevant information, such that a robust GAE model is able to accurately predict from the last set of codes (last hidden layer), the original raw data (data reconstruction). In our analysis, the computational task was to predict the original cytokine data and use age as a second output variable, such that the predicted values represent a given individuals’ age-related chronic inflammation level, or inflammatory clock.
To test the robustness and quality of the GAE method, we compared the accuracy of the age prediction against other widely used dimensionality reduction methods that use linear equations, such as the elastic net and principal component analysis (PCA), as well as those involving non-linear equations, such as plain auto-encoders and neural networks (Fig. S3a and b). Overall, the GAE method outperformed other methods in predicting chronological age (P < 0.05) with the exception of the comparison with a plain neural network (P = 0.54) (Fig. S3b). These results indicate that the phenomenon of low-grade chronic inflammation in aging humans is best modeled using non-linear methods, and based on these, one can derive a metric for chronic inflammation that accurately predicts chronological age in the population, while preserving the biological information related to the total inflammatory burden as measured by the level of circulating immune proteins.
.../...
.
Edited by Engadin, 28 November 2019 - 07:36 PM.









































