A new study describes a novel anti-cancer vaccine based on antigen-producing bacteria that can tackle solid and metastatic cancers [1].
Invading an invader
Years ago, scientists discovered that bacteria can colonize tumors [2]. Some bacteria are drawn to the tumor microenvironment due to factors such as necrotic tissue, hypoxia, and nutrient availability. For example, Clostridium species prefer anaerobic conditions and have been explored in tumor-targeting therapies. Salmonella and E. coli strains have also shown an affinity for tumors [3].
This led to the idea of a microbial anti-cancer vaccine: using tumor-targeting bacteria to improve an organism’s immune response to cancer. However, this task has proven to be difficult. In a new study published in Nature, researchers from Columbia University report creating a sophisticated bacterial vector that is effective against solid tumors, which are considered particularly tough targets.
Takes out cancer, including metastatic
It takes several mutations to turn a healthy cell into a cancerous one. The products of those mutations, which might include full-length mutated proteins and truncated protein chains, can elicit an immune response (become antigens).
The researchers identified several such “neoantigens” in a type of colorectal carcinoma and genetically engineered E. coli to produce them in large quantities. Mice were then inoculated with cancer cells. After tumors developed, the bacterial vaccine was injected directly into the tumor microenvironment.
The bacteria readily colonized the tumors but not healthy tissues. As expected, tumor antigens produced by the bacteria elicited a strong, multi-faceted immune response. A single injection effectively prevented tumor growth, with three out of seven mice exhibiting a complete response (full tumor eradication).
The researchers then complicated the task: the mice were inoculated with cancer cells on both sides of the body, leading to the appearance of two tumors. Only one tumor was treated with the bacterial vaccine to see if this could produce a systemic response.
As the researchers hoped, the treatment produced a sustained systemic immune response. The bacteria were only found in the treated tumors, but the untreated tumors also came under attack by the immune system.
Injecting a drug directly into the tumor can be complicated, so the researchers tried intravenous delivery. They found that the bacteria were quickly cleared away from healthy tissues but successfully colonized the tumor and produced results comparable to intratumoral administration.
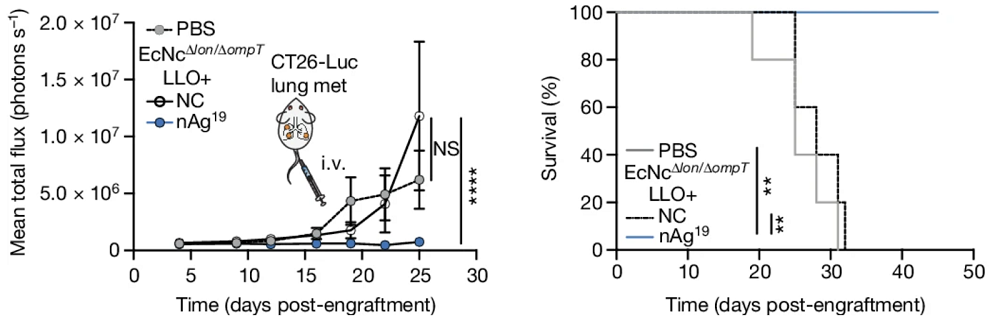
Another tough test was metastases. Metastatic (stage 4) cancers are virtually incurable. In this study, lung metastases were created by injecting carcinoma cells into the bloodstream. After the engraftment, the bacterial vaccine was also injected intravenously. Amazingly, all the treated animals survived past day 50 of the experiment, while all the animals in the other groups succumbed to cancer much earlier.
The researchers then tackled a more aggressive tumor cell type (B16F10 melanoma). Of course, they had to engineer a new strain of bacteria carrying melanoma-specific antigens. The treatment produced strong results with localized tumors, blocking their growth almost completely. With metastatic melanoma, the survival rate was 60% in the treatment group versus zero in the control group.
A bespoke treatment
According to the authors, their modified bacteria “recruit and activate dendritic cells, stimulate both neoantigen-specific and broad adaptive immunity, and reduce immunosuppression within the tumor microenvironment.” The researchers also predict that their system might produce a synergistic effect when combined with other treatments.
The new therapy would have to be tailored not only to a specific type of cancer but to each patient. “The time to treatment will first depend on how long it takes to sequence the tumor,” said Tal Danino, associate professor of biomedical engineering at Columbia’s School of Engineering and a leading author on the study. “Then we just need to make the bacterial strains, which can be quite fast. Bacteria can be simpler to manufacture than some other vaccine platforms.”
However, there’s an upside to that level of personalization. Since the vaccine is based on several tumor-specific antigens, the cancer will hardly be able to evade it by rapidly mutating. “Because our platform allows us to deliver so many different neoantigens, it theoretically becomes difficult for tumor cells to lose all those targets at once and avoid the immune response,” said another leading author, Nicholas Arpaia, associate professor of microbiology and immunology at Columbia University’s Vagelos College of Physicians and Surgeons.
Literature
[1] Redenti, A., Im, J., Redenti, B., Li, F., Rouanne, M., Sheng, Z., Sun, W., Gurbatri, C. R., Huang, S., Komaranchath, M., Jang, Y., Hahn, J., Ballister, E. R., Vincent, R. L., Vardoshivilli, A., Danino, T., & Arpaia, N. (2024). Probiotic neoantigen delivery vectors for precision cancer immunotherapy. Nature, 1-9.
[2] Yu, Y. A., Zhang, Q., & Szalay, A. A. (2008). Establishment and characterization of conditions required for tumor colonization by intravenously delivered bacteria. Biotechnology and bioengineering, 100(3), 567-578.
[3] Pawelek, J. M., Low, K. B., & Bermudes, D. (1997). Tumor-targeted Salmonella as a novel anticancer vector. Cancer research, 57(20), 4537-4544.
View the article at lifespan.io









































