A novel therapy based on induced neuronal stem cells shows promise in a mouse model of Alzheimer’s disease – and it can be administered intranasally [1].
Who needs cells?
Stem cell therapies have made great strides in recent decades. They have been successfully employed against numerous diseases, from cancer to osteoarthritis. However, storing, transporting, and administering cells is not easy. Moreover, in some cases, cells, with their extraordinarily complex metabolisms, can produce unwanted side effects. For instance, neural stem/progenitor cells (NSCs) have been shown to improve symptoms of certain brain diseases [2] but can also trigger pathological changes in the brain [3].
However, the whole cell might not always be necessary. Cells have been known to communicate with each other by excreting extracellular vesicles (EVs), tiny membrane-bound bubbles that can carry various cargoes, such as RNA molecules and proteins. Scientists have learned to harvest vesicles produced by cells and administer them locally or systemically, often recapitulating much of the effect of cell administration.
Unlike stem cells, EVs can be frozen and thawed without compromising their therapeutic efficacy. Furthermore, cells of different types can now be easily produced from induced pluripotent stem cells (iPSCs). Those are somatic cells reverted into pluripotency by applying certain molecules, such as the original reprogramming cocktail of Yamanaka factors (OSKM).
Less inflammation
In a new study published in the Journal of Extracellular Vesicles, researchers from Texas A&M University took human iPSCs and re-differentiated them into NSCs. They then harvested the extracellular vesicles produced by the cells, purified them, and administered them intranasally to a mouse model of familial Alzheimer’s disease (5xFAD mice). Despite decades of research and tens of billions of dollars spent, a cure for Alzheimer’s remains elusive.
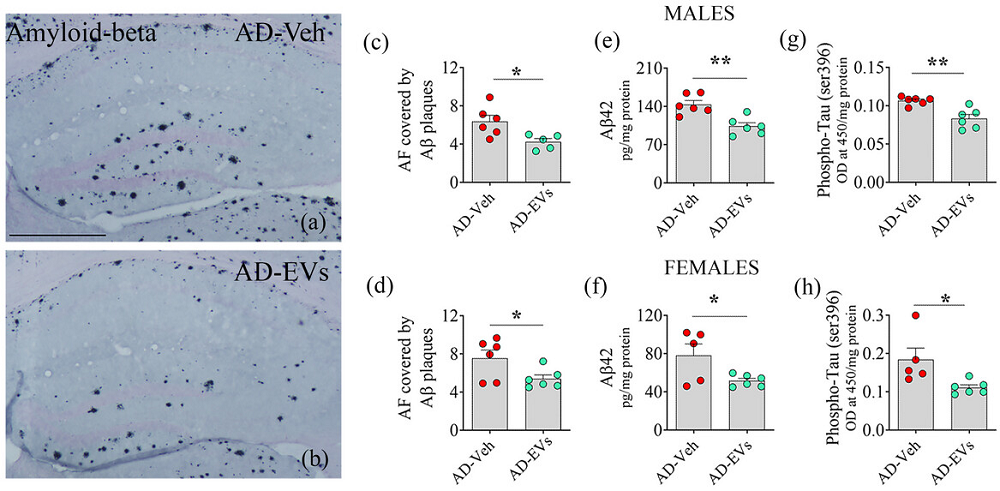
While mouse models of Alzheimer’s have their limitations, as mice naturally don’t develop this disease, 5xFAD mice have been widely used. These animals start displaying Alzheimer’s-like pathologies, such as amyloid beta (Aβ) plaques and increased neuroinflammation at the age of three months, which is when the treatment was administered. About two months later, the mice underwent cognitive and neuropathological assessments.
The researchers confirmed that the EVs were indeed taken up by the brain’s resident macrophages (microglia). In Alzheimer’s, these cells surround Aβ plaques, presumably in an attempt to remove them. They display increased activation and inflammation, which has been linked to disease progression.
“Prolonged activation causes microglia to lose their normal function and begin to harm neurons, leading to progressive neuron loss,” explains Ashok K. Shetty, Ph.D., a University Distinguished Professor and associate director at the Institute for Regenerative Medicine in the Department of Cell Biology and Genetics, and the corresponding author on the study.
RNA sequencing revealed that the treatment downregulated multiple inflammation-related pathways that were significantly upregulated in 5xFAD mice compared to healthy controls. Notably, this occurred without compromising the microglia’s phagocytosis function: their ability to engulf and destroy pathogens.
The treatment also led to a significant reduction in the burden of Aβ plaques and phosphorylated tau protein, two major hallmarks of Alzheimer’s. While both sexes showed improvements, males demonstrated a more robust response to the treatment.
By the age of five months, 5xFAD mice typically demonstrate significant cognitive decline, which was also observed in this study. The EV treatment, however, appeared to effectively block this decline. Tests included the object location test, in which cognitively healthy animals are expected to spend more time exploring an object in a novel place than in a familiar place, and the pattern recognition test, which measures the ability to discern novel objects from familiar ones.
Interestingly, the researchers also assessed the mice’s mood. Mood changes are increasingly gaining recognition as a clinically important aspect of Alzheimer’s disease. Just like many human Alzheimer’s patients, untreated 5xFAD mice exhibited anhedonia, the inability to enjoy things – in this case, sweetened water. The EV treatment restored the rodents’ joie de vivre – or at least their preference for sugar.
Similar effects in human cells
While the researchers did not test their treatment in human patients, they pursued the next best alternative: applying NSC-derived EVs to human microglia in vitro. When challenged with Aβ-42, an isoform of Aβ known for its high aggregation propensity and central role in the pathology of Alzheimer’s disease, microglia exhibited overactivation and an inflammatory phenotype. These effects, however, were reversed by the EV treatment.
According to the paper, EVs are superior to NSCs in that they do not replicate and readily cross the blood-brain barrier. Intranasal administration is easy, non-invasive, and characterized by rapid action. While the study was conducted on animals at early stages of the disease, constant advances in diagnostics make this less of a limitation.
“This approach is effective because the cargo carried by these extracellular vesicles could reduce the neuropathological changes in the brain,” says Shetty, who has filed a patent on the intranasal application of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and other neurological disorders. “Our journey to advance the application of this therapy for Alzheimer’s disease is just beginning.”
Literature
[1] Madhu, L. N., Kodali, M., Upadhya, R., Rao, S., Somayaji, Y., Attaluri, S., … & Shetty, A. K. (2024). Extracellular vesicles from human‐induced pluripotent stem cell‐derived neural stem cells alleviate proinflammatory cascades within disease‐associated microglia in Alzheimer’s disease. Journal of Extracellular Vesicles, 13(11), e12519.
[2] Temple, S. (2023). Advancing cell therapy for neurodegenerative diseases. Cell stem cell, 30(5), 512-529.
[3] Abdi, S., Javanmehr, N., Ghasemi-Kasman, M., Bali, H. Y., & Pirzadeh, M. (2022). Stem cell-based therapeutic and diagnostic approaches in Alzheimer’s disease. Current Neuropharmacology, 20(6), 1093-1115.









































