A recent study linked probiotic-induced gut microbiome and metabolite changes to improved muscle functioning in older sarcopenia patients [1].
Sarcopenia and the gut
Sarcopenia is an age-related condition. People with sarcopenia suffer from a reduction in muscle mass, strength, and function, leading to a decreased quality of life and increased morbidity and mortality [2].
The authors of this study, citing evidence of a link between the gut microbiome, muscle health, and sarcopenia, investigated the effect of the consumption of a probiotic on the muscle health of sarcopenia patients. They used Bifidobacterium animalis subsp. Lactis Probio-M8 (Probio-M8), a probiotic strain present in human breast milk [3]. Probio-M8 has already been shown to have a positive impact on bone metabolism [4] and in the treatment of Parkinson’s disease in older adults [5].
Anti-aging effects in mice
The researchers administered Probio-M8 to 19-month-old mice for 28 days. They observed improved muscle function and a significant reduction in senescence in the mice that received probiotics, suggesting an anti-aging effect.
The researchers also investigated inflammatory markers but didn’t see significant differences between the treatment and control groups. They suggest that this might be due to existing low inflammation in the control group, which does not allow probiotic treatment to lower it further.
Impact on microbes and metabolites
The impact of probiotic treatment on the structure and diversity of the gut microbiome in old mice was limited. A deeper look into the 10 most populous bacterial species in these groups’ fecal matter revealed a pathogen (Mucispirillum schaedleri) that was far more abundant in the control group. Previous reports suggested that this microbe may cause ulcerative colitis [6]. This is in contrast to probiotic-treated mice, in which the researchers observed abundant beneficial microbes.
There were also beneficial changes in the metabolites in the fecal and serum samples of old mice treated with the probiotic. The treatment led to a significant increase in anti-inflammatory, anticancer, and antioxidant metabolites, metabolites that have been reported to have benefits against aging, and metabolites that may somewhat alleviate neurological disorders, such as Alzheimer’s disease and Parkinson’s disease.
The chair test
The promising results in mice led to a test of this probiotic on 43 older sarcopenia patients. Following 60 days of supplementation with Probio-M8, the researchers observed a roughly 16% reduction in the five-time chair stand (FTCS) test time among the treated patients. This test requires patients to sit and stand up five times and measures lower limb strength. This significant result suggests an improvement in overall physical performance.
However, other sarcopenia-related measurements didn’t support the optimistic results obtained in the FTCS test. Skeletal muscle mass, grip strength, calf circumference, and BMI didn’t significantly change following the probiotic treatment.
Additionally, an evaluation of multiple physiological sarcopenia-related measurements showed mostly no changes compared to controls, except for reduced total cholesterol.
The role of microbial metabolites
Similarly to the results obtained in mice, human samples also showed modest changes in the richness and structure of the gut microbiome after probiotic treatment. Some of the most significant changes included increased numbers of beneficial gut bacteria, and reduced numbers of pathogenic gut bacteria, in patients with sarcopenia.
Despite modest changes in microbial composition, the researchers observed significant metabolite changes: the probiotic treatment enriched the microbial pathways involved in vitamin C biosynthesis and nucleotide metabolism. The researchers suggest that higher activity of those pathways might play a role in microbes’ support for host antioxidant defenses and nucleotide availability.
Other metabolites that were increased in feces and serum are involved in anti-inflammatory effects and processes essential for vital physiological functions, or they are associated with skeletal muscle, such as metabolites promoting the proliferation of skeletal muscle cells. There was also an increase in a compound that is considered a source of muscle energy and important for promoting muscle protein synthesis: creatine.
The researchers noted that the impact of the probiotic treatment on the composition of the gut microbiome was modest. However, the impact on the metabolite changes was significant, leading them to further investigations into how probiotic-driven metabolite changes influence host physical performance.
A series of bioinformatic analyses and models were employed to identify key players in the connection between Probio-M8 and sarcopenia. The authors summarized that their analysis “suggests that Probio-M8 may positively influence muscle metabolism, potentially through its effects on the gut microbiome and subsequent modulation of creatine synthesis or utilization.”
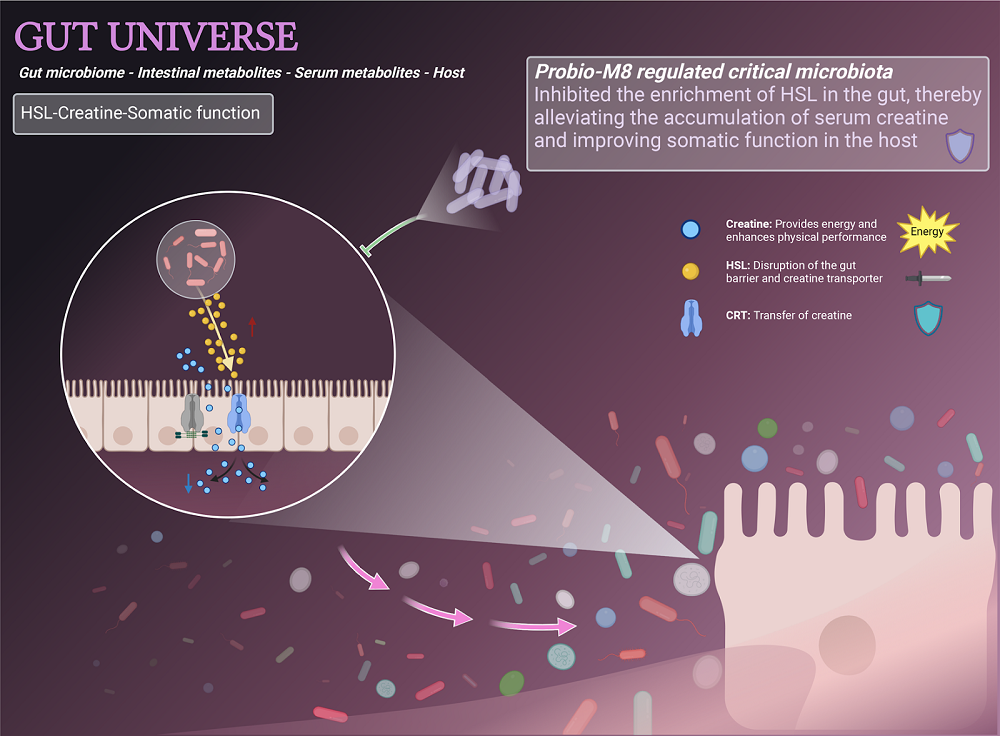
A computational analysis of metabolites also pointed the researchers toward a hypothesis that one of the harmful molecules known as n-dodecyl-l-homoserine lactone (HSL) “could reduce the absorption of creatine from the gut.” To test this, they created a cell culture monolayer of enterocytes. Enterocytes are intestinal absorptive cells that are located on the inner surface of the small and large intestines. An experiment confirmed that HSL interfered with creatine transport by affecting the level of its transporter (CRT).
Molecular understanding
In the discussion section, the researchers gathered the molecular evidence that they and others presented to assemble a possible mechanism of action.
One of the key players appears to be creatine, and these researchers have found that this probiotic encourages creatine to be delivered into the bloodstream from the gut. Creatine is a compound essential for muscles and, when combined with resistance training, can increase lean mass and muscle strength in older adults. Previous research suggested that creatine supplementation has benefits in older adults with sarcopenia [7]. The authors suggest that creatine might “act as a buffer to inhibit the production of reactive oxygen species (ROS) by serving as a neutralizing agent.” The inhibition of ROS is important, since accumulation of ROS has been linked to muscle function and muscle loss [8].
Probio-M8 can inhibit the enrichment of HSL in patients with sarcopenia, thereby promoting the accumulation of creatine in the serum and improving the host’s overall physical performance.
Literature
[1] Zhang, Z., Fang, Y., He, Y., Farag, M. A., Zeng, M., Sun, Y., Peng, S., Jiang, S., Zhang, X., Chen, K., Xu, M., Han, Z., & Zhang, J. (2024). Bifidobacterium animalis Probio-M8 improves sarcopenia physical performance by mitigating creatine restrictions imposed by microbial metabolites. NPJ biofilms and microbiomes, 10(1), 144.
[2] Cohen, S., Nathan, J. A., & Goldberg, A. L. (2015). Muscle wasting in disease: molecular mechanisms and promising therapies. Nature reviews. Drug discovery, 14(1), 58–74.
[3] Zhong, Z., Tang, H., Shen, T., Ma, X., Zhao, F., Kwok, L. Y., Sun, Z., Bilige, M., & Zhang, H. (2022). Bifidobacterium animalis subsp. lactis Probio-M8 undergoes host adaptive evolution by glcU mutation and translocates to the infant’s gut via oral-/entero-mammary routes through lactation. Microbiome, 10(1), 197.
[4] Zhao, F., Guo, Z., Kwok, L. Y., Zhao, Z., Wang, K., Li, Y., Sun, Z., Zhao, J., & Zhang, H. (2023). Bifidobacterium lactis Probio-M8 improves bone metabolism in patients with postmenopausal osteoporosis, possibly by modulating the gut microbiota. European journal of nutrition, 62(2), 965–976.
[5] Sun, H., Zhao, F., Liu, Y., Ma, T., Jin, H., Quan, K., Leng, B., Zhao, J., Yuan, X., Li, Z., Li, F., Kwok, L. Y., Zhang, S., Sun, Z., Zhang, J., & Zhang, H. (2022). Probiotics synergized with conventional regimen in managing Parkinson’s disease. NPJ Parkinson’s disease, 8(1), 62.
[6] Kuffa, P., Pickard, J. M., Campbell, A., Yamashita, M., Schaus, S. R., Martens, E. C., Schmidt, T. M., Inohara, N., Núñez, G., & Caruso, R. (2023). Fiber-deficient diet inhibits colitis through the regulation of the niche and metabolism of a gut pathobiont. Cell host & microbe, 31(12), 2007–2022.e12.
[7] Casciola, R., Leoni, L., Cuffari, B., Pecchini, M., Menozzi, R., Colecchia, A., & Ravaioli, F. (2023). Creatine Supplementation to Improve Sarcopenia in Chronic Liver Disease: Facts and Perspectives. Nutrients, 15(4), 863.
[8] Watson, M. D., Cross, B. L., & Grosicki, G. J. (2021). Evidence for the Contribution of Gut Microbiota to Age-Related Anabolic Resistance. Nutrients, 13(2), 706.








































