A big fat debate
#61
Posted 30 January 2010 - 11:43 PM
http://coolinginflam...s-linoleic.html
Bottom-line: PUFAs are the most dangerous fats to (over)consume, right behind trans fats.
#62
Posted 31 January 2010 - 01:37 AM
Renamed this thread to ensure no one thinks it's focused against MR. The real enemy are inflammatory PUFAs, after all. (And, in fact, while PUFAs are a necessary fat, they should not be promoted as heart-healthy, nrt necessary healthy at all -- they are ONLY okay in moderation, and in proportion to omega-3's.) More on this here:
http://coolinginflam...s-linoleic.html
Bottom-line: PUFAs are the most dangerous fats to (over)consume, right behind trans fats.
Hummmm. It's another pretty confusing issue. If you look at the paper he referenced at the end of his post, there does not seem to be a lot of studies that found that n-6 correlate with an increase in CHD risk. If anything, they reduce it.
Actually, many review to date found that modifying/reducing total fat intake is not a great mean of reducing CHD risk, so it's certainly probable that n-6 don't influence it that much either.
It might be time to focus less on these kind of detail and just make sure to get wholesome food, high quality food, control caloric intake, make sure you're not overweight, practice exercise, have majorly a plant-based diet (veggies) with emphasis on raw/slightly cook vegetable - and probably around half of protein quantity from plant source.
Thinking about this, all of the promoter of the "n-6 is the demon" have never fournish very solid scientic evidence about it. (it's mainly speculation about how n-6 might promote inflammation & oxidation)
I'm hoping we can come to a conclusion about this soon.
I'd like it to be settle
Edited by oehaut, 31 January 2010 - 01:40 AM.
#63
Posted 31 January 2010 - 02:21 AM
i think i will stick to MUFAs as my main fat source and chicken/beef for proteinHummmm. It's another pretty confusing issue. If you look at the paper he referenced at the end of his post, there does not seem to be a lot of studies that found that n-6 correlate with an increase in CHD risk. If anything, they reduce it.The real enemy are inflammatory PUFAs, after all. (And, in fact, while PUFAs are a necessary fat, they should not be promoted as heart-healthy, nrt necessary healthy at all -- they are ONLY okay in moderation, and in proportion to omega-3's.) More on this here:
http://coolinginflam...s-linoleic.html
Bottom-line: PUFAs are the most dangerous fats to (over)consume, right behind trans fats.
Actually, many review to date found that modifying/reducing total fat intake is not a great mean of reducing CHD risk, so it's certainly probable that n-6 don't influence it that much either.
Edited by Michael, 31 January 2010 - 12:57 PM.
Trim quotes
#64
Posted 31 January 2010 - 04:14 AM
In human studies, higher plasma levels of omega-6 PUFAs, mainly AA, were associated with decreased plasma levels of serum proinflammatory markers, particularly interleukin-6 and interleukin-1 receptor antagonist, and increased levels of antiinflammatory markers, particularly transforming growth factor-ß.18 When healthy volunteers were given ~7 times the usual intake of AA (ie, 1.5 g/d) in a 7-week controlled feeding study, no effects on platelet aggregation, bleeding times, the balance of vasoactive metabolites, serum lipid levels, or immune response were observed.5–8
Diets high in LA can increase the ex vivo susceptibility of low-density lipoprotein (LDL) to oxidation,21 and oxidized LDL can promote vascular inflammation.22 Therefore, oxidized LDL may play some role in the etiology of CHD.23 However, the extent of LDL oxidation at higher LA intakes (5% to 15% of energy) has not been established, and its clinical relevance is in question owing to the general failure of antioxidant treatments to mitigate CHD risk in most randomized trials.24 At present, little direct evidence supports a net proinflammatory, proatherogenic effect of LA in humans.22,25,26
In a meta-analysis of 25 case-control studies (including 1998 cases and 6913 controls) evaluating blood/tissue omega-6 PUFA content and CHD events, LA content was inversely associated with CHD risk, whereas AA was unrelated to CHD risk.
These observational studies use the strongest designs, minimizing both selection and recall bias. No significant associations between LA or omega-6 PUFA intake and CHD risk were seen in the Finnish Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study,40 Lipid Research Clinics study,41 or Honolulu Heart Program.42 Modest, nonsignificant inverse associations were observed in the Multiple Risk Factor Intervention Trial,43 the Irish-Boston Heart Study,44 and the Health Professionals Follow-Up Study.45 In the Health Professionals Follow-Up Study, CHD rates were lowest in participants with higher intake of both omega-3 and omega-6 PUFAs,46 and in the Western Electric Study47 and the Kupio Heart Study,48 higher LA intakes or serum levels were associated with lower risk of CHD or total mortality. In the Nurses’ Health Study, in which diet was assessed multiple times over 20 years,49 CHD risk was ~25% lower comparing the 95th and 5th percentiles of LA intake (7.0% versus 2.8% of energy, respectively). Most prospective cohort studies have not found significant associations between omega-6 fatty acid intakes and ischemic50 –52 or hemorrhagic50,51,53 stroke or stroke mortality.54
Nevertheless, not all studies support a beneficial effect of LA on CHD risk markers. For example, an angiographic study reported a direct association between PUFA intakes and luminal narrowing in women with CHD.33 However, effects on markers do not always translate into effects on actual clinical end points; thus, it is essential to evaluate the relations between LA consumption and CHD events.
Could it just be that n-6 are not bad? There certainly must be something if MR think so... I doubt he has any conflict of interest about this.
But the last point is interesting. It would be a good thing to have more study done using clinical end points such as coronary angiography. In the Mozaffarian et al. study, PUFAs was positively correlated with progression (p=0.04)
Edited by Michael, 31 January 2010 - 01:00 PM.
Formatting
#65
Posted 31 January 2010 - 03:38 PM
What is the American Heart Association’s Agenda? —It Sure Ain’t Science or Public Health
Blog... not peer-reviewed... but still, she had written a letter to Circulaton Editor, which will not be published for reason given in the comments section of the rebuttal.
Where is the Science? The Science Advisory on Omega-6 Polyunsaturated Fats
Evelyn Tribole
CIRCULATIONAHA/2009/868448
There are several sweeping claims, based on research taken out of context. This letter highlights only a few of the problems.
Harris et al.[1] cite a series of metabolic studies in which healthy men were fed a diet high in arachidonic acid (AA) and claim there was no evidence of harmful effects [2]. Yet, that’s not what the data show.
When the men ate a high AA diet (1.5 grams/day), they experienced a marked increase in AA-derived vasoactive compounds, compared to when they ate a stabilizing diet with 210 mg/d of AA. There was 41% more thromboxane (TXA2), a powerful inducer of platelet aggregation and vasoconstriction and 27% more prostacyclin, compared to their baseline levels. The researchers called this magnitude of increase “remarkable” and concluded that increasing dietary AA could increase the risk of thrombosis [2].
The selective omission of this conclusion is especially troubling, given that most cases of myocardial infarction are due to the formation of an occluding thrombus on the surface of the arterial plaque. [3] Also problematic, is the size and duration of this study series, which had only 10 subjects, who were fed the high AA diet for a net of a 50-day period--hardly a basis from which to generalize help orharm to the public.
Ferrucci’s inChianti study was cited as another example of no harm, because the subjects with the highest (AA) blood levels had lower pro-inflammatory markers and higher anti-inflammatory markers [4]. Once again, an important detail is ignored—the subjects from this Mediterranean region of Italy eat a low omega-6 PUFA diet, averaging 7 grams of total PUFA/day.
In this context, it is not surprising that plasma AA was associated with beneficial inflammation biomarkers--because it does so in the presence of eating a low omega-6 diet, providing 3 percent of energy from omega-6 PUFA. Yet, the AHA advisory urges nearly double this amount of omega-6 fat for Americans of at least 5% to10% of energy from omega-6 PUFAs (12 grams for women and 17 grams for men).
AHA’s advisory continues the problematic trend identified by Tricoci et al [5], which found that a large proportion of recommendations in ACC/AHA guidelines are based on the lowest category of evidence, “expert” opinion, in formulating guidelines with little empirical evidence. Health care professionals are well-advised to heed Tricoci’s recommendation--to exercise caution when considering guidelines not supported by solid evidence, which unfortunately is the case with this omega-6 PUFA advisory.
References
1. Harris WS, Mozaffarian D, Rimm E, Kris-Etherton P, Rudel LL, Appel LJ, Engler MM, Engler
MB, Sacks F. Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the
American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity,
and Metabolism; Council on Cardiovascular Nursing; and Council on Epidemiology and Prevention.
Circulation. 2009 Feb 17; 119(6): 902-907.
2. Ferretti A, Nelson GJ,Schmidt PC, Kelley DS, Bartolini G, and Flanagan VP . Increased Dietary
Arachidonic Acid Enhances the Synthesis of Vasoactive Eicosanoids in Humans. Lipids, 1997; 32,
435–439.
3. Hansson, G. Mechanisms of disease Inflammation, Atherosclerosis, and Coronary Artery Disease.
New England Journal of Medicine. 2005;352:1685-95.
4. Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F, Martin A, Andres-Lacueva
C, Senin U, and Guralnik JM. Relationship of plasma polyunsaturated fatty acids to circulating
inflammatory markers, J. Clin. Endocrinol. Metab. 91 (2006) 439–446.
5. Tricoci P, Allen JM, Kramer JM, Califf RM, and Smith SC. Practice Guidelines Scientific
Evidence Underlying the ACC/AHA Clinical Practice Guidelines. JAMA. 2009;301(8):831-841.
Things are getting pretty bad if we cannot even trust a review from a scientific comittee in a peer-reviewed journal. Personally, I don't have time to review everything myself. I'll certainly read this reference #5.
Edited by oehaut, 31 January 2010 - 03:47 PM.
#66
Posted 31 January 2010 - 05:07 PM
But often times the researchers in these studies draw conclusions based on false premises. For example, the majority of the medical community adheres to the mistaken notion that LDL is bad, and therefore anything that lowers it is good. Turns out, oils rich in PUFAs do in fact lower LDL. So, when these researchers see LDL fall, they conclude that PUFA-rich oils are heart healthy.Renamed this thread to ensure no one thinks it's focused against MR. The real enemy are inflammatory PUFAs, after all. (And, in fact, while PUFAs are a necessary fat, they should not be promoted as heart-healthy, nrt necessary healthy at all -- they are ONLY okay in moderation, and in proportion to omega-3's.) More on this here:
http://coolinginflam...s-linoleic.html
Bottom-line: PUFAs are the most dangerous fats to (over)consume, right behind trans fats.
Hummmm. It's another pretty confusing issue. If you look at the paper he referenced at the end of his post, there does not seem to be a lot of studies that found that n-6 correlate with an increase in CHD risk. If anything, they reduce it.
Actually, many review to date found that modifying/reducing total fat intake is not a great mean of reducing CHD risk, so it's certainly probable that n-6 don't influence it that much either.
It might be time to focus less on these kind of detail and just make sure to get wholesome food, high quality food, control caloric intake, make sure you're not overweight, practice exercise, have majorly a plant-based diet (veggies) with emphasis on raw/slightly cook vegetable - and probably around half of protein quantity from plant source.
Thinking about this, all of the promoter of the "n-6 is the demon" have never fournish very solid scientic evidence about it. (it's mainly speculation about how n-6 might promote inflammation & oxidation)
I'm hoping we can come to a conclusion about this soon.
I'd like it to be settle
Whoops!!!!
It's this sort of thinking that had led us down so many wrong paths in dietary science.
Edited by DukeNukem, 31 January 2010 - 05:08 PM.
#67
Posted 31 January 2010 - 07:10 PM
Things are getting pretty bad if we cannot even trust a review from a scientific comittee in a peer-reviewed journal. Personally, I don't have time to review everything myself.
But the whole debate is whether the consensus is wrong. Nobody denies that the AHA's position is to eat more PUFAs, so it's not surprising that they are willing to publish reviews that attempt to support their position. We are claiming that that position is incorrect, at least vis a vis PUFA restriction to 3% of energy and n-3/n-6 PUFA balance (between 1:1 and 1:4).
#68
Posted 31 January 2010 - 08:12 PM
We are claiming that that position is incorrect, at least vis a vis PUFA restriction to 3% of energy and n-3/n-6 PUFA balance (between 1:1 and 1:4).
Yes, but we need solid scientific proof to make such a claim. This is what i'm after. I'd like to find a comprehensive review of why n-6 are bad. (much like this one, but supporting the contrary opinion)
#69
Posted 31 January 2010 - 10:49 PM
We are claiming that that position is incorrect, at least vis a vis PUFA restriction to 3% of energy and n-3/n-6 PUFA balance (between 1:1 and 1:4).
Yes, but we need solid scientific proof to make such a claim. This is what i'm after. I'd like to find a comprehensive review of why n-6 are bad. (much like this one, but supporting the contrary opinion)
Agreed.
#70
Posted 02 February 2010 - 07:48 AM
Am J Clin Nutr. 2004 Nov;80(5):1175-84.
Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women.
Mozaffarian D, Rimm EB, Herrington DM.
Channing Laboratory, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Harvard School of Public Health, Boston, Massachusetts, USA. dmozaffa@hsph.harvard.edu
Erratum in:
Am J Clin Nutr. 2005 Jan;81(1):199.
Comment in:
Am J Clin Nutr. 2004 Nov;80(5):1102-3.
...In multivariate analyses, a higher saturated fat intake was associated with a smaller decline in mean minimal coronary diameter (P = 0.001) and less progression of coronary stenosis (P = 0.002) during follow-up. Compared with a 0.22-mm decline in the lowest quartile of intake, there was a 0.10-mm decline in the second quartile (P = 0.002), a 0.07-mm decline in the third quartile (P = 0.002), and no decline in the fourth quartile (P < 0.001); P for trend = 0.001. .... Monounsaturated and total fat intakes were not associated with progression. CONCLUSIONS: In postmenopausal women with relatively low total fat intake, a greater saturated fat intake is associated with less progression of coronary atherosclerosis, whereas carbohydrate intake is associated with a greater progression.
PMID: 15531663 [PubMed - indexed for MEDLINE]
Higher saturated fat intake is associated with regression of the plaque.
However since oxLDL is associated with athersclerosis this study found that increasing MUFA and decreasing SFA decreased oxLDL and macrophage uptake:
Br J Nutr. 2008 Sep;100(3):569-75. Epub 2008 Jan 29.
A monounsaturated fatty acid-rich diet reduces macrophage uptake of plasma oxidised low-density lipoprotein in healthy young men.
Moreno JA, López-Miranda J, Pérez-Martínez P, Marín C, Moreno R, Gómez P, Paniagua JA, Pérez-Jiménez F.
CIBER Fisiopatologia Obesidad y Nutricion, Instituto de Salud Carlos III, Spain.
During atherogenesis, a pathological accumulation of lipids occurs within aortic intimal macrophages through uptake of plasma oxidised LDL (oxLDL). The aim of the present study was to determine whether macrophage uptake of plasma oxLDL and LDL susceptibility to oxidation may be determined by quantity and quality of dietary fat. Twenty healthy young men were subjected to three dietary periods, each lasting 4 weeks. The first was an SFA-enriched diet (38 % fat, 20 % SFA), which was followed by a carbohydrate (CHO)-rich diet (30 % fat, < 10 % SFA, 55 % CHO) or a MUFA olive oil-rich diet (38 % fat, 22 % MUFA) following a randomised cross-over design. After each diet period, LDL particles were oxidised with Cu ions to determine LDL susceptibility to oxidation and subsequently incubated with the U937-macrophage cell line to determine the percentage of uptake of plasma oxLDL. The shift from the MUFA diet to the SFA- or CHO-rich diets reduced the resistance of LDL particles to oxidation, decreasing lag time (P = 0.038) and increasing the propagation rate (P = 0.001). Furthermore, the MUFA-rich diet demonstrated reduced macrophage uptake of plasma oxLDL (P = 0.031) as compared with the SFA-rich diet. Finally, macrophage uptake of plasma oxLDL was correlated (r 0.45; P = 0.040) with total amount of conjugated dienes after LDL oxidation. Our data suggest that a MUFA-rich diet may have favourable effects on cardiovascular risk since it prevents the oxidative modifications of LDL and reduces macrophage uptake of plasma oxLDL.
PMID: 18226292 [PubMed - indexed for MEDLINE]
It seems through mechanistic evidence MUFA is best however looking at the endpoints SFA may be best. Maybe 1:1 ratio is safest for now.
Also regarding PUFAs here's a good review:
Biochem Pharmacol. 2009 Mar 15;77(6):937-46. Epub 2008 Oct 28.
Dietary n-6 and n-3 polyunsaturated fatty acids: from biochemistry to clinical implications in cardiovascular prevention.
Russo GL.
Institute of Food Sciences, National Research Council, 83100 Avellino, Italy. glrusso@isa.cnr.it
Linoleic acid (LA) and alpha linolenic acid (ALA) belong to the n-6 (omega-6) and n-3 (omega-3) series of polyunsaturated fatty acids (PUFA), respectively. They are defined "essential" fatty acids since they are not synthesized in the human body and are mostly obtained from the diet. Food sources of ALA and LA are most vegetable oils, cereals and walnuts. This review critically revises the most significant epidemiological and interventional studies on the cardioprotective activity of PUFAs, linking their biological functions to biochemistry and metabolism. In fact, a complex series of desaturation and elongation reactions acting in concert transform LA and ALA to their higher unsaturated derivatives: arachidonic acid (AA) from LA, eicosapentaenoic (EPA) and docosahexaenoic acids (DHA) from ALA. EPA and DHA are abundantly present in fish and fish oil. AA and EPA are precursors of different classes of pro-inflammatory or anti-inflammatory eicosanoids, respectively, whose biological activities have been evoked to justify risks and benefits of PUFA consumption. The controversial origin and clinical role of the n-6/n-3 ratio as a potential risk factor in cardiovascular diseases is also examined. This review highlights the important cardioprotective effect of n-3 in the secondary prevention of sudden cardiac death due to arrhythmias, but suggests caution to recommend dietary supplementation of PUFAs to the general population, without considering, at the individual level, the intake of total energy and fats.
PMID: 19022225 [PubMed - indexed for MEDLINE]
It mentions this article:
Biomed Pharmacother. 2002 Oct;56(8):365-79.
The importance of the ratio of omega-6/omega-3 essential fatty acids.
Simopoulos AP.
The Center for Genetics, Nutrition and Health, Washington, DC 20009, USA. cgnh@bellatlantic.net
Several sources of information suggest that human beings evolved on a diet with a ratio of omega-6 to omega-3 essential fatty acids (EFA) of approximately 1 whereas in Western diets the ratio is 15/1-16.7/1. Western diets are deficient in omega-3 fatty acids, and have excessive amounts of omega-6 fatty acids compared with the diet on which human beings evolved and their genetic patterns were established. Excessive amounts of omega-6 polyunsaturated fatty acids (PUFA) and a very high omega-6/omega-3 ratio, as is found in today's Western diets, promote the pathogenesis of many diseases, including cardiovascular disease, cancer, and inflammatory and autoimmune diseases, whereas increased levels of omega-3 PUFA (a low omega-6/omega-3 ratio) exert suppressive effects. In the secondary prevention of cardiovascular disease, a ratio of 4/1 was associated with a 70% decrease in total mortality. A ratio of 2.5/1 reduced rectal cell proliferation in patients with colorectal cancer, whereas a ratio of 4/1 with the same amount of omega-3 PUFA had no effect. The lower omega-6/omega-3 ratio in women with breast cancer was associated with decreased risk. A ratio of 2-3/1 suppressed inflammation in patients with rheumatoid arthritis, and a ratio of 5/1 had a beneficial effect on patients with asthma, whereas a ratio of 10/1 had adverse consequences. These studies indicate that the optimal ratio may vary with the disease under consideration. This is consistent with the fact that chronic diseases are multigenic and multifactorial. Therefore, it is quite possible that the therapeutic dose of omega-3 fatty acids will depend on the degree of severity of disease resulting from the genetic predisposition. A lower ratio of omega-6/omega-3 fatty acids is more desirable in reducing the risk of many of the chronic diseases of high prevalence in Western societies, as well as in the developing countries, that are being exported to the rest of the world.
PMID: 12442909 [PubMed - indexed for MEDLINE]
That shows data that in Japanese people the AA content is similiar to those in Western people however the Omega 3's are higher in the Japanese, so maybe Omega 6 content doesn't matter regarding heart disease. However I am a proponent of the Paleo Principles and will stick to lowering n-6 and increasing n-3 (it just makes so much sense
Edited by Sillewater, 02 February 2010 - 07:53 AM.
#71
Posted 02 February 2010 - 06:27 PM
Unquestionably, marine/animal omega-3's (unlike the plant version, ALA) reduce the inflammatory effect of omega-6's -- often dramatically. But, likely not fully, and this "solution" is not as foolproof as simply reducing omega-6's as a preventative measure. Especially all processed omega-6s, which NEVER existed until 100 years ago, and we did pretty well without them up until then.That shows data that in Japanese people the AA content is similiar to those in Western people however the Omega 3's are higher in the Japanese, so maybe Omega 6 content doesn't matter regarding heart disease. However I am a proponent of the Paleo Principles and will stick to lowering n-6 and increasing n-3 (it just makes so much sense
)
(This opens the door for the nim-wits among us to retort: "But wait! Life spans increased since 100 years ago!" I look forward to ignoring this entirely uneducated counter-claim.)
#72
Posted 08 February 2010 - 06:31 PM
#73
Posted 08 February 2010 - 07:54 PM
In some cases yes, such as with unprocessed olive oil (well, even EVOO has some processing, but extremely minimal) and tea oil (I don't mean tea tree oil).As with the polyphenol content of olive oil, could it be that vegetable oil brings in good amount of antioxidants and that could be an important confounding factor in the epidemiology?
But, if we had, for example, EV corn oil, or EV soy oil, these oils would contain polyphenols but still be a huge net negative, IMO. Likewise, no one ever recommends processed olive oil, because the processing -- usually heat is involved -- not only destroys some portion of the polyphenols, but also oxidizes a portion of the oil.
Processed oil = bad. This is an excellent rule of thumb, with perhaps no exceptions.
Not to mention most vegetable oils contain >10% PUFAs, which creates an inflammatory environment inside our body. The latest study backing this up.
Edited by DukeNukem, 08 February 2010 - 07:54 PM.
#74
Posted 12 February 2010 - 06:11 AM
#75
Posted 12 February 2010 - 03:22 PM
MR are his initials.
Edited by Shepard, 12 February 2010 - 03:37 PM.
#76
Posted 12 February 2010 - 09:09 PM
Renamed this thread to ensure no one thinks it's focused against MR. The real enemy are inflammatory PUFAs, after all. (And, in fact, while PUFAs are a necessary fat, they should not be promoted as heart-healthy, nrt necessary healthy at all -- they are ONLY okay in moderation, and in proportion to omega-3's.) More on this here:
http://coolinginflam...s-linoleic.html
Bottom-line: PUFAs are the most dangerous fats to (over)consume, right behind trans fats.
To say vegetable oil is bad is one thing, how about all the nutritional content of nuts? Pecans, Almonds and such surely cannot be treated with the same disdain for omega-6 fats.
#77
Posted 12 February 2010 - 11:14 PM
To say vegetable oil is bad is one thing, how about all the nutritional content of nuts? Pecans, Almonds and such surely cannot be treated with the same disdain for omega-6 fats.
I think most of the concern is for vegetable oils like soybean, corn, and rapeseed (aka canola) since they make up a larger part of the typical American diet than oil from nuts.
#78
Posted 12 February 2010 - 11:24 PM
Habitual Dietary Intake of n-3 and n-6 Fatty Acids in Relation to Inflammatory Markers Among US Men and Women
"These results suggest that n-6 fatty acids do not inhibit the antiinflammatory effects of n-3 fatty acids and that the combination of both types of fatty acids is associated with the lowest levels of inflammation. The inhibition of inflammatory cytokines may be one possible mechanism for the observed beneficial effects of these fatty acids on chronic inflammatory-related diseases."
Interestingly, regarding the stance of the AHA:
"The AHA report also addresses the recent controversy that omega-6 fatty acids, via linoleic acid, which accounts for 85-90% of dietary omega-6, may actually increase inflammation and thereby increase rather than reduce cardiovascular risk. Any link between omega-6 and inflammation, says the AHA, comes from the fact that arachidonic acid, which can be formed from linoleic acid, is involved in the early stages of inflammation, but anti-inflammatory molecules are also formed; these suppress the production of adhesion molecules, chemokines and interleukins, all of which are key mediators of the atherosclerotic process. Thus, concludes the report, it is incorrect to view the omega-6 fatty acids as pro-inflammatory." [source]
I think the AHA might be looking at the issue too simplistically, particularly with their recommendation of 5-10% of calories from n-6 PUFA. Instead of quantity, the AHA should specify ratio, specific pathology, and genetic predisposition as most important:
The importance of the ratio of omega-6/omega-3 essential fatty acids
"Several sources of information suggest that human beings evolved on a diet with a ratio of omega-6 to omega-3 essential fatty acids (EFA) of
 1 whereas in Western diets the ratio is 15/1–16.7/1. Western diets are deficient in omega-3 fatty acids, and have excessive amounts of omega-6 fatty acids compared with the diet on which human beings evolved and their genetic patterns were established. Excessive amounts of omega-6 polyunsaturated fatty acids (PUFA) and a very high omega-6/omega-3 ratio, as is found in today's Western diets, promote the pathogenesis of many diseases, including cardiovascular disease, cancer, and inflammatory and autoimmune diseases, whereas increased levels of omega-3 PUFA (a low omega-6/omega-3 ratio) exert suppressive effects. In the secondary prevention of cardiovascular disease, a ratio of 4/1 was associated with a 70% decrease in total mortality. A ratio of 2.5/1 reduced rectal cell proliferation in patients with colorectal cancer, whereas a ratio of 4/1 with the same amount of omega-3 PUFA had no effect. The lower omega-6/omega-3 ratio in women with breast cancer was associated with decreased risk. A ratio of 2–3/1 suppressed inflammation in patients with rheumatoid arthritis, and a ratio of 5/1 had a beneficial effect on patients with asthma, whereas a ratio of 10/1 had adverse consequences. These studies indicate that the optimal ratio may vary with the disease under consideration. This is consistent with the fact that chronic diseases are multigenic and multifactorial. Therefore, it is quite possible that the therapeutic dose of omega-3 fatty acids will depend on the degree of severity of disease resulting from the genetic predisposition. A lower ratio of omega-6/omega-3 fatty acids is more desirable in reducing the risk of many of the chronic diseases of high prevalence in Western societies, as well as in the developing countries, that are being exported to the rest of the world."
1 whereas in Western diets the ratio is 15/1–16.7/1. Western diets are deficient in omega-3 fatty acids, and have excessive amounts of omega-6 fatty acids compared with the diet on which human beings evolved and their genetic patterns were established. Excessive amounts of omega-6 polyunsaturated fatty acids (PUFA) and a very high omega-6/omega-3 ratio, as is found in today's Western diets, promote the pathogenesis of many diseases, including cardiovascular disease, cancer, and inflammatory and autoimmune diseases, whereas increased levels of omega-3 PUFA (a low omega-6/omega-3 ratio) exert suppressive effects. In the secondary prevention of cardiovascular disease, a ratio of 4/1 was associated with a 70% decrease in total mortality. A ratio of 2.5/1 reduced rectal cell proliferation in patients with colorectal cancer, whereas a ratio of 4/1 with the same amount of omega-3 PUFA had no effect. The lower omega-6/omega-3 ratio in women with breast cancer was associated with decreased risk. A ratio of 2–3/1 suppressed inflammation in patients with rheumatoid arthritis, and a ratio of 5/1 had a beneficial effect on patients with asthma, whereas a ratio of 10/1 had adverse consequences. These studies indicate that the optimal ratio may vary with the disease under consideration. This is consistent with the fact that chronic diseases are multigenic and multifactorial. Therefore, it is quite possible that the therapeutic dose of omega-3 fatty acids will depend on the degree of severity of disease resulting from the genetic predisposition. A lower ratio of omega-6/omega-3 fatty acids is more desirable in reducing the risk of many of the chronic diseases of high prevalence in Western societies, as well as in the developing countries, that are being exported to the rest of the world."
Edited by Skotkonung, 12 February 2010 - 11:26 PM.
#79
Posted 18 February 2010 - 11:03 PM
Note, it's likely not just corn oil that'll have this effect, it's any oil high in PUFAs. In other words, the exact oils that the AHA loves to recommend as "heart healthy." Never mind the bones, though!Dissolve Away those Pesky Bones with Corn Oil
CO [corn oil] is known to promote bone loss, obesity, impaired glucose tolerance, insulin resistance and thus represents a useful model for studying the early stages in the development of obesity, hyperglycemia, Type 2 diabetes [23] and osteoporosis. We have used omega-6 fatty acids enriched diet as a fat source which is commonly observed in today's Western diets basically responsible for the pathogenesis of many diseases [24].
http://wholehealthso...bones-with.html
(And, the heart part is kinda wrong, too.)
#80
Posted 01 March 2010 - 08:22 AM
http://www.ncbi.nlm....pubmed/19948181
Coenzyme Q addition to an n-6 PUFA-rich diet resembles benefits on age-related mitochondrial DNA deletion and oxidative stress of a MUFA-rich diet in rat heart.
Quiles JL, Pamplona R, Ramirez-Tortosa MC, Naudí A, Portero-Otin M, Araujo-Nepomuceno E, López-Frías M, Battino M, Ochoa JJ.
Institute of Nutrition and Food Technology José Mataix Verdú, Department of Physiology, University of Granada, Granada, Spain. jlquiles@ugr.es
Age-related changes in cardiomyocytes reduce the capacity to recover from acute injury or to adapt during chronic disease in advanced age. N-6 polyunsaturated fatty acids (n-6PUFA) lead to higher lipid peroxidation during aging than the less oxidizable monounsaturated fatty acids (MUFA); and coenzyme Q (CoQ)-supplemented n-6PUFA lengthens the lifespan and reduces peroxidation in comparison to non-supplemented n-6PUFA. Here, lifelong feeding on MUFA, n-6PUFA, and n-6 PUFA+CoQ was compared regarding age-related alterations in rat heart. Less mitochondrial area and perimeter were reported for aged n-6 PUFA-fed animals while MUFA led to a higher density of mitochondrial cristae. Mitochondrial complexes and cytochrome c oxidase activity decreased with aging (except complex I and cytochrome c oxidase in n-6 PUFA+CoQ), while increased apoptosis-inducing factor was found with aging. MUFA led to lower mitochondrial DNA-deletion frequency. The lowest hydroperoxide levels for aged animals were found for n-6 PUFA+CoQ, which also showed lower concentrations than did n-6 PUFA. For protein oxidation, specific carbonyl compounds were lower in aged animals; meanwhile lipoxidation-derived protein-oxidation markers were higher. The results suggest that MUFA can protect mitochondria from age-related changes, and that CoQ supplementation to n-6 PUFA partially resembles MUFA benefits. Moreover, under our experimental conditions, lipid-derived oxidative damage appears to be more important than the pure protein-derived oxidative damage during aging.
#81
Posted 01 March 2010 - 01:01 PM
anyone ever read this study or have a thought?
http://www.ncbi.nlm....pubmed/19948181
This is one of the reasons that I think claims about "optimal diets" are pretty much bunk, and why I don't subscribe to any particular dieting ideology. Everyone is different and supplementation vastly changes the effects of dieting. Normal healthy people should just stick to the basics... lots of veggies, not too much sugar, don't smoke, don't drink excessively (or at all), get proper sleep, some basic supplementation, and exercise.
Older people have more to gain with more expensive supps like CoQ10 and hardcore diets like CR, IF, methionine restriction, and such. Perhaps if I were older I would look into a high fat diet... but I would definitely try to get at least 50% of my fat from MUFAs.
I wouldn't rule out all PUFA though... heck Omega 3s are PUFA. Duke's constant generalizations are probably harmful to the diet ideology he is trying to spread.
Edited by progressive, 01 March 2010 - 01:05 PM.
#82
Posted 01 March 2010 - 06:20 PM
Duke's constant generalizations are probably harmful to the diet ideology he is trying to spread.
I'm noticing he tends to do that a lot...
I don't see what anyone can actually learn from sweeping declaratives, conjecture, anecdotes, etc.
Edited by Xanthus, 01 March 2010 - 06:26 PM.
#83
Posted 11 March 2010 - 04:56 PM
Associations between diet, lifestyle factors, and telomere length in women
Background: Leukocyte telomere length is associated with diseases of aging, but there is limited knowledge of diet and lifestyle determinants
Objective: The objective was to examine cross-sectionally the association between diet, body composition, and lifestyle factors on leukocyte telomere length in women.
Design: Leukocyte telomere length was measured by quantitative polymerase chain reaction in 2284 female participants from the Nurses' Health Study, who were selected as controls for an investigation of biological predictors of cancer. Diet, lifestyle, and anthropometric data were assessed by questionnaire.
Results: After multivariate adjustment, dietary fiber intake was positively associated with telomere length (z score), specifically cereal fiber, with an increase of 0.19 units between the lowest and highest quintiles (P = 0.007, P for trend = 0.03). Although total fat intake was not associated with telomere length, polyunsaturated fatty acid intake (–0.26 units, quintile 5 compared with quintile 1: P = 0.002, P for trend = 0.02), specifically linoleic intake, was inversely associated with telomere length after multivariate adjustment (–0.32 units; P = 0.001, P for trend = 0.05). Waist circumference was inversely associated with telomere length [0.15-unit difference in z score in a comparison of the highest (≥32 in, 81.28 cm) with the lowest (≤28 in, 71.12 cm) category (P = 0.01, P for trend = 0.02) in the multivariate model]. We found no association between telomere length and smoking, physical activity, or postmenopausal hormone use.
Conclusions: Although the strength of the associations was modest in this population of middle- and older-age women, our results support the hypothesis that body composition and dietary factors are related to leukocyte telomere length, which is a potential biomarker of chronic disease risk.
Could it be then that PUFA-6 reduce lifespan?
Edited by oehaut, 11 March 2010 - 04:58 PM.
#84
Posted 13 March 2010 - 12:05 AM
Did you see this:Looking at the article in press from AJCN, I saw that one out yesterday.
Associations between diet, lifestyle factors, and telomere length in womenBackground: Leukocyte telomere length is associated with diseases of aging, but there is limited knowledge of diet and lifestyle determinants
Objective: The objective was to examine cross-sectionally the association between diet, body composition, and lifestyle factors on leukocyte telomere length in women.
Design: Leukocyte telomere length was measured by quantitative polymerase chain reaction in 2284 female participants from the Nurses' Health Study, who were selected as controls for an investigation of biological predictors of cancer. Diet, lifestyle, and anthropometric data were assessed by questionnaire.
Results: After multivariate adjustment, dietary fiber intake was positively associated with telomere length (z score), specifically cereal fiber, with an increase of 0.19 units between the lowest and highest quintiles (P = 0.007, P for trend = 0.03). Although total fat intake was not associated with telomere length, polyunsaturated fatty acid intake (–0.26 units, quintile 5 compared with quintile 1: P = 0.002, P for trend = 0.02), specifically linoleic intake, was inversely associated with telomere length after multivariate adjustment (–0.32 units; P = 0.001, P for trend = 0.05). Waist circumference was inversely associated with telomere length [0.15-unit difference in z score in a comparison of the highest (≥32 in, 81.28 cm) with the lowest (≤28 in, 71.12 cm) category (P = 0.01, P for trend = 0.02) in the multivariate model]. We found no association between telomere length and smoking, physical activity, or postmenopausal hormone use.
Conclusions: Although the strength of the associations was modest in this population of middle- and older-age women, our results support the hypothesis that body composition and dietary factors are related to leukocyte telomere length, which is a potential biomarker of chronic disease risk.
Could it be then that PUFA-6 reduce lifespan?
Peroxidation of linoleic acid and its relation to aging and age dependent diseases.
"Cell proliferation, cell injury and aging are connected with changes in the cell membrane structure. Apparently these changes activate, in mammalian as well as in plant cells, lipases which liberate polyunsaturated fatty acids (PUFAs). PUFAs are the substrates for lipoxygenases which convert them to corresponding hydroperoxides (LOOHs). Lipoxygenases commit suicide by releasing iron ions. LOOHs react with iron ions to generate radicals. Thus, a nonenzymic lipid peroxidation process (LPO) is induced. It is speculated that the change from enzymic to nonenzymic LPO is connected with the switch from apoptosis to necrosis and that LOOHs produced in enzymic reactions are degraded specifically to signal compounds which induce physiological responses, while nonenzymic reactions seem to induce generation of reactive oxygen species, cell death and age related diseases. Enzymic and nonenzymic LPO processes concern all PUFAs not only arachidonic acid. The main PUFA in mammals is linoleic acid. Since these products serve signalling functions, different degradation paths of linoleic-hydroperoxides are described in detail and the physiological properties of LPO products are discussed in relation to aging and age related diseases."
Dual mechanisms for telomerase inhibition in DLD-1 human colorectal adenocarcinoma cells by polyunsaturated fatty acids
"Polyunsaturated fatty acids (PUFAs) have been reported to have antitumor activity. In this study, we have tested whether telomerase might be a target for the antitumor effect of fatty acids using DLD-1 colorectal adenocarcinoma cells. In a cell-free approach, fatty acids were added directly to cell lysates, and we confirmed that increasing fatty acid unsaturation correlates with increased inhibition of telomerase activity. Using a cell culture approach, DLD-1 cells were cultured with fatty acids. In a time and dose dependent manner, EPA and DHA suppressed cellular telomerase activity and the mRNAs encoding hTERT (human telomerase reverse transcriptase) and c-myc. Based on these observations, we suggest that PUFAs inhibit telomerase activity through dual mechanisms: direct inhibition of enzymatic activity and down regulation of hTERT, one of the telomerase components."
High PUFA diet could lead to accelerated aging via telomerase inhibition but less incidence of cancer?
Edited by Skotkonung, 13 March 2010 - 12:08 AM.
#85
Posted 13 March 2010 - 09:31 PM
There is good evidence that a low PUFA diet (especially when n-3/n-6 balanced) can prevent cancer (Lyon Diet Heart Study, Another human trial, Corn oil/mouse study).
If PUFAs (n-3 or n-6) have a role in treating cancer, it is likely due to their propensity to oxidize as certain pro-oxidants seem to discriminately kill cancer cells. It's the same theory behind the use of high dose intravenous vitamin C, selenite, or vitamin k3 in treating cancers. However, I wouldn't assume that these things prevent cancer - just as I wouldn't assume chemotherapy prevents cancer.
Edited by Jay, 13 March 2010 - 09:49 PM.
#86
Posted 08 April 2013 - 06:09 PM
http://www.ncbi.nlm....pubmed/23386268
But as far as I understand the PUFAs were processed oils. So I don't think that we can make conclusions about saturated fats being better than nuts based on this study.
#87
Posted 08 April 2013 - 08:23 PM
Replacing Saturated Fats with omega6-PUFAs increases all-cause mortality:
http://www.ncbi.nlm....pubmed/23386268
But as far as I understand the PUFAs were processed oils. So I don't think that we can make conclusions about saturated fats being better than nuts based on this study.
Thanks for the update DAMI. This is a good debate and more data is needed.
#88
Posted 08 April 2013 - 08:53 PM
Replacing Saturated Fats with omega6-PUFAs increases all-cause mortality:
http://www.ncbi.nlm....pubmed/23386268
But as far as I understand the PUFAs were processed oils. So I don't think that we can make conclusions about saturated fats being better than nuts based on this study.
Thanks for the update DAMI. This is a good debate and more data is needed.
I wonder how much more data it will take? That was a pretty damning study, considering that substituting PUFA for SAFA is religion in the cardiac community. The PUFA group looked worse even on CHD metrics, not to mention all-cause mortality! That wasn't the first time PUFAs came up looking bad, either. One thing to bear in mind is that this was a secondary prevention cohort. They were only looking at people who had already had a heart attack. Primary prevention, that is, trying to prevent the first CHD event, could be different, though based on the only metrics I care about, which are all-cause, it probably won't be; at least not wildly.
#89
Posted 08 April 2013 - 08:59 PM
Replacing Saturated Fats with omega6-PUFAs increases all-cause mortality:
http://www.ncbi.nlm....pubmed/23386268
But as far as I understand the PUFAs were processed oils. So I don't think that we can make conclusions about saturated fats being better than nuts based on this study.
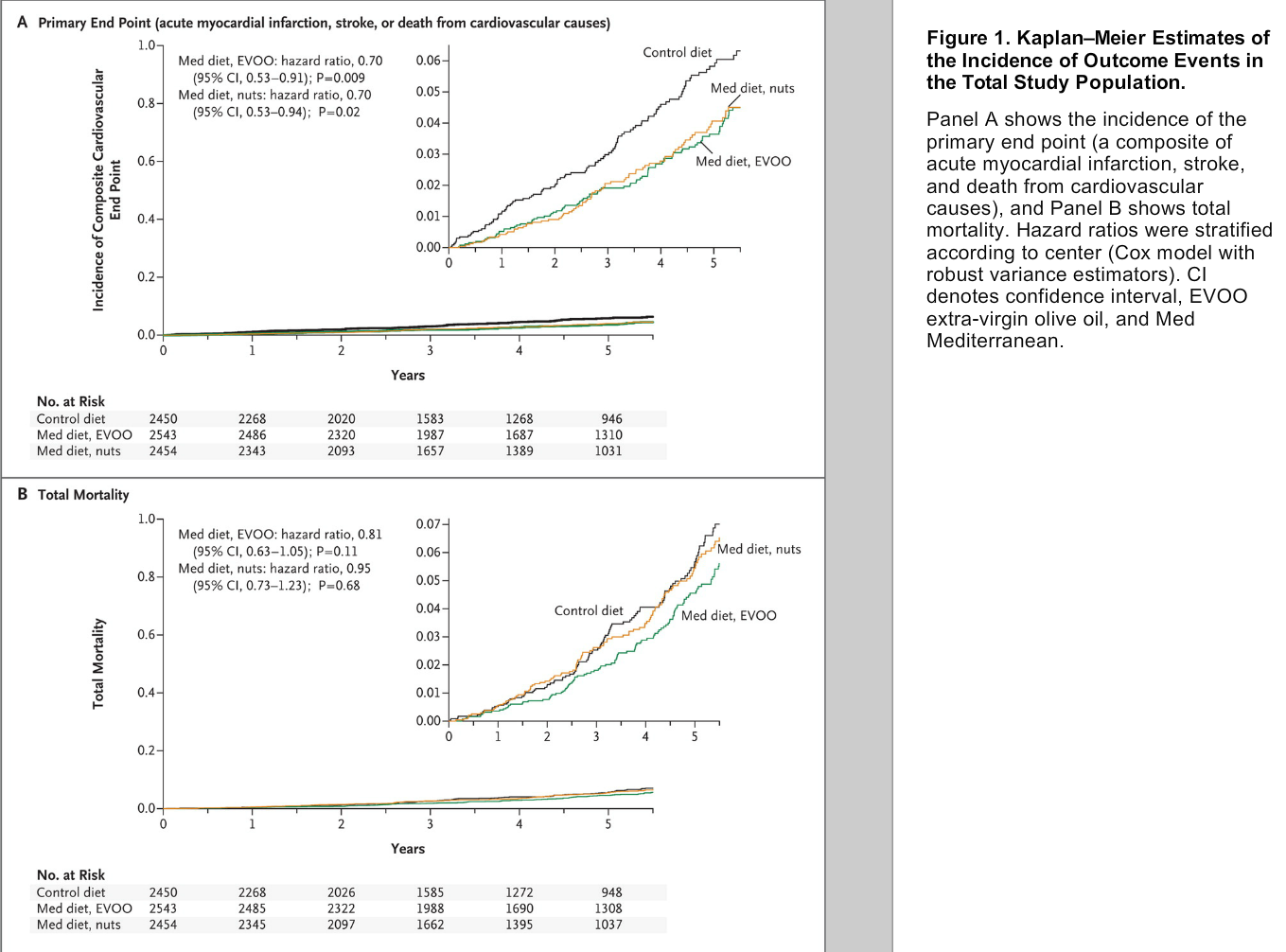
Whole nuts might not be much better than the processed oils. In this study, both olive oil and nuts reduced cardiovascular disease deaths by the same amount compared to control. The people given nuts however, still had an all-cause mortality as high as the control, which means they were dying of something else at an increased rate. More PUFAs leading to more lipid peroxides leading to more cancer perhaps?
#90
Posted 09 April 2013 - 04:51 PM
For saturated fat, I no longer avoid it like the plague like so many so-called experts advise. There seems to be enough epidemiological evidence to not be worried, IMO.
Nice to see a few new studies from time-to-time though.
6 user(s) are reading this topic
0 members, 6 guests, 0 anonymous users