So, to start, I strongly endorse Sköt's suggestions that you cut down your fruit intake, and get some legumes into you. I also agree that you need to eat more fat, tho' not SAFA (more on this below); can you please post your macronutrient ratios from the COM pie graph? Either post or PM or email me, and I'll edit them into your post.
I'm also a bit concerned about the specific PATTERN of your fruit intake (almost always alone, in large quantities): all that sugar with no protein or fat really isn't a good thing for your liver and postprandial insulin and lipids.
I agree that you (and, really, everyone who isn't eating a huge amount of liver or a variety of fatty fish, and isn't a Damned Fool about sun exposure) need to supplement vitamin D, and get yourself tested. OTOH, I really don't think you need to worry about your vitamin A levels: sure, you get no preformed retinol, but you're getting
45 times the RDA, for chrissake! Your conversion rate can't possibly be that poor, or you'd be long since have gone blind.
Also, the widespread notion, often repeated even in the scientific literature, that we need to get dietary EPA & DHA because ALA conversion rates are 'poor.' This is a mechanistically-based, make-the-case
petitio principii, which
assumes that some higher rate is necessary, finds that it's lower, and gets worried, despite the overwhelming evidence that
ALA conversion to EPA and DHA is adequate to ensure cardiovascular and other health outcomes. And, you (Sthira) are getting
lots of ALA. As well, there's good reason to think that
people on CR should minimize dietary EPA, DHA, & fish oil.
Similarly, the belief that dietary saturated fat is 'necessary' based on its better support of HDL levels is also mechanistically backward, and again rebutted by the evidence from
actual health outcomes. There are now several meta-analyses of prospective epidemiology and clinical trials (1-3) all showing that substitution of saturated with polyunsaturated fat (but not, importantly, with carbohydrate) leads to better cardiovascular health outcomes. This conclusion actually very likely underestimates the strength of the effect, in part because in many of the included studies, the 'low' SaFA diets still contained way too damned much saturated fat (should be ≤7% of energy), and the high intake of carbohydrate (esp. high-GI carb (see eg. (4)) and prevalence of overweight and obesity and ensuing insulin resistance (see studies by Volek and by others), and other reasons to think that
the evidence that saturated fat really is bad for you probably underestimate the true strength of their effect.
I think the evidence on this is clear, and have no intention of
re-litigating this subject, NB. However, I will (with some trepidation) address some of Sköt's specific issues.
First, the easy one: HDL. Plenty of mono fats -- combined with cutting back the sugar -- should, IAC, deal with low HDL cholesterol. But a better question would be: Sthira, I know you get tested; are you happy with your HDL levels? IF not, another good reason to get yourself some olive oil!
Now, the harder ones:
Intake of certain fatty acids may increase cholesterol levels, but again this is more consistent with greater cholesterol synthesis. For example the most powerful increaser of total cholesterol is probably lauric acid, but lauric acid is also the most powerful reducer of the LDL-to-HDL-cholesterol ratio -- this is consistent with lauric acid being burned for quick energy, thus increasing the energy state of the liver cell and allowing for greater cholesterol synthesis. Not "blocking" the LDL receptor or anything nefarious like that.
This is, again, a mechanistically-based argument. It is unfortunately difficult to do proper, prospective epidemiological studies on
actual health outcomes associated with consumption of individual fatty acids, and esp lauric acid, because it's such a minor contributor to total SFA intake and in most populations is too strongly correlated with same; however, (5) did indeed find a small increase in CHD risk with each SaFA individually from lauric (12:0) to stearic (18:0). Notably, these subjects were free of not only atherosclerosis, but even
hypercholesterolemia, when the study began.
For mechanism addicts can indulge their habits with (6-10), and
here and
here; but really, this is all speculative, vs. the well-supported generalized evidence that lowering
SaFA as a class in favor of PUFA is protective against negative cardiovascular outcomes.
Fat composition in the diet changes the composition / oxidation of the lipoprotein. PUFAs may lower LDL, but simply having a low LDL level may not be enough to be protective against CVD. Experimental evidence has shown in humans that saturated fats protect against in vivo LDL oxidation. You can see this by looking at the rightward most column in this graph: Dietary Fat and LDL Oxidation. This shows a graded increase in LDL oxidation occuring within the blood of live humans as the diet goes from 1) butter and palm oil to 2) olive oil to 3) sunflower oil and finally 4) sunflower oil and fatty fish, all diets being about 35% of calories from fat.
You have to be really, really careful when you look at studies of LDL oxidation. Notably, this study does not show that dietary saturated fats protect against
in vivo LDL
oxidation: it shows that dietary saturated fats "protect" against
ex vivo LDL
peroxidizability. They are not the same thing, even tho' abstracts sometimes assert "LDL oxidation" without qualification. They did not measure actual,
in vivo oxidized LDL levels: they extracted LDL out of the body, and then assessed "Lag time of Cu2+-oxidated LDL" and "Conjugated dienes in Cu2+-oxidated LDL." Ie, they soaked them in unphysiologic levels of copper ions, and induced the Fenton reaction. Surprise! You get lipid peroxidation. This doesn't reflect the in vivo situatioin at all, at all.
Unfortunately, while at least a few studies have confirmed that replacing carb with mono fat lowers
in vivo LDL oxidation, only one study that I've been able to find tested a high-MUFA diet against a high-SaFA diet -- and it's a graduate thesis, still unpublished, and in Spanish, and in insulin-resistant subjects.(11) However, it did indeed find that a high-MUFA (mostly from olive oil) diet lowered
in vivo postprandial oxidized LDL relative to a high-SaFA one (mixed sources, but a lot of butter). You'd likely need a longer time period to meaningfully assay typical basal oxLDL levels.
After the initial selection of volunteers and obtaining informed consent, the 11 participants, randomly and in a Latin square crossover design for Williams, followed by three dietary periods of 28 days duration: one rich in SAT fat to a composition of 47% CHO, 15% protein and 38% fat (23% SAT, 9% Mono, 6% poly), another low in fat and high in CHO consisting of 65% CHO, 15% protein and 20% fat (6% SAT, 8% and 6% POLY MONO) and a third rich in mono with 47% CHO, 15% protein and 38% fat (9% SAT, 23% and 6% POLY MONO), then all patients were treated, sequentially, the other two diets up to a total of 12 weeks. ... The design of the experimental diets was based on the replacement of fat SAT CHOC in low-fat diet while in the high-fat diet, the fat MONO replaced the SAT ...
The postprandial expression of messenger ribonucleic acid (mRNA) of UCP2 in the peripheral adipose tissue was higher after the CHO diet. Postprandial concentrations of glucose and insulin increased after the meal high in HC while free fatty acids (FFAs) increased after high-fat diets. The levels of total cholesterol, triglycerides and low density lipoprotein (LDL) did not change during the three phases of diet, whereas cholesterol high density lipoprotein (HDL) decreased after the diet high in CHO. Postprandial concentration of LDL-ox decreased after ingestion of the MONO diet and serum NT [nitrotyrosine] levels increased after ingestion of a diet rich in CHO.(11)
 Figure 14. Representation of the mean values ​​of LDL-ox baseline and at 60, 120 and 180 minutes of breakfast. ANOVA for repeated measures. *P <0.05, **p <0.01.
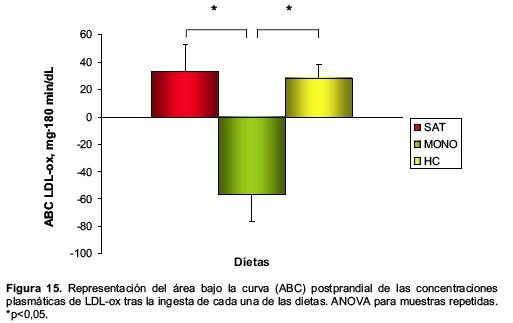
Figure 14. Representation of the mean values ​​of LDL-ox baseline and at 60, 120 and 180 minutes of breakfast. ANOVA for repeated measures. *P <0.05, **p <0.01.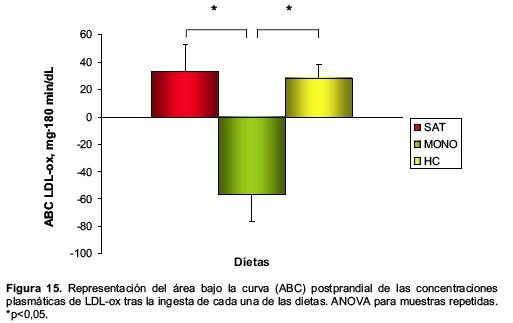 Figure 15. Representing the area under the curve (AUC) postprandial plasma concentrations of LDL-ox after ingestion of each of the diets. ANOVA for repeated measures. *P <0.05.
Figure 15. Representing the area under the curve (AUC) postprandial plasma concentrations of LDL-ox after ingestion of each of the diets. ANOVA for repeated measures. *P <0.05.But, again, in evaluating the effect of diet on health outcomes, one should rely on the long-term, prospective epidemiology and clinical trials
with health outcomes, not these make-the-case, mechanistically-based speculations.
Similarly, I have little concern about intake of nonessential amino acids, granted that you're getting well over the RDA for total protein, and at least the RDA for individual
essential aminos. (Remember that you have to add Met + Cys to get the %RDA for S-containing aminos. More legumes should deal with your marginal lysine intake).
Again, similarly, I wouldn't arbitrarily conclude that any given Calorie intake may be too little. Just as it's impossible to define what is "enough" CR or the "%CR" of any given person, I don't think one can say
a priori that someone is consuming 'too few' Calories -- esp just based on hir height, w/o knowing hir weight or anthropometry. The questions are: is his weight stable? Does he feel good? Is he subjectively healthy? Does his bloodwork look reassuring? If you hit all the checklists, an arbitrary idea of how many Calories one 'needs' (or how one should not go below some 'minimum' BMI) is not grounded in evidence.
References1: Mozaffarian D, Micha R, Wallace S.
Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010 Mar 23;7(3):e1000252. Review. PubMed PMID: 20351774; PubMed Central PMCID: PMC2843598.
2: Skeaff CM, Miller J.
Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55(1-3):173-201. Epub 2009 Sep 15. PubMed PMID: 19752542.
3: Jakobsen MU, O'Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A.
Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009 May;89(5):1425-32. Epub 2009 Feb 11. PubMed PMID: 19211817; PubMed Central PMCID: PMC2676998.
4: Jakobsen MU, Dethlefsen C, Joensen AM, Stegger J, Tjønneland A, Schmidt EB, Overvad K. Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr. 2010 Jun;91(6):1764-8. Epub 2010 Apr 7. PubMed PMID: 20375186.
5. Hu FB, Stampfer MJ, Manson JE, Ascherio A, Colditz GA, Speizer FE, Hennekens CH, Willett WC.
Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr. 1999 Dec;70(6):1001-8.
PMID: 10584044 [PubMed - indexed for MEDLINE]
6: Tholstrup T. Influence of stearic acid on hemostatic risk factors in humans. Lipids. 2005 Dec;40(12):1229-35. PubMed PMID: 16477807.
7: Fernandez ML, West KL. Mechanisms by which dietary fatty acids modulate plasma lipids. J Nutr. 2005 Sep;135(9):2075-8. Review. PubMed PMID: 16140878.
8: Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003 May;77(5):1146-55. PubMed PMID: 12716665.
9: Steer P, Vessby B, Lind L. Endothelial vasodilatory function is related to the proportions of saturated fatty acids and alpha-linolenic acid in young men, but not in women. Eur J Clin Invest. 2003 May;33(5):390-6. PubMed PMID: 12713452.
10: Temme EH, Mensink RP, Hornstra G. Effects of diets enriched in lauric, palmitic or oleic acids on blood coagulation and fibrinolysis. Thromb Haemost. 1999 Feb;81(2):259-63. PubMed PMID: 10064003.
11: Sánchez García, María Esther, Juan Antonio.
Efectos de tres modelos de dieta sobre la expresión de UCP-2 en tejido adiposo periférico y marcadores de oxidación en pacientes con resistencia a la insulina. 2008; Universidad de Córdoba. Servicio de Publicaciones.
http://helvia.uco.es...andle/10396/325
Edited by Michael, 15 December 2013 - 04:29 PM.