Protracted benzo withdrawal and Gotu Kola, Piracetam, Bacopa
#91
Posted 16 September 2012 - 01:34 AM
Thanks for the reply. Yeah I think Kompota is right too. I've read some articles talking about how the receptors become blunted in a sense and no longer respond to GABA. Also, they talk about BZD receptors coupling with GABAR and how that could be the cause as well. Honestly, I'm not so sure that GABAR agonists would make the PAWS symptoms worse. I mean think about it... have you ever heard of someone complaining of PAWS from valerian use? And also, if what I said is true about the coupling of the GABA and BZD receptors, then most likely only further use of benzos would exacerbate symptoms.
Anyhow, yeah I wish the inverse agonists were on the market. I would really love to try them...
So if there is a conformational change to the receptor, what do we do about it? Besides flumazenil or one of the inverse agonists... An NMDA antagonist might help in the meantime. Acamprosate for example. I say this because since the GABAR do not respond to GABA properly, glutamate runs rampant and has a merry old excitable time. An NMDA antagonist could help. Also, take a look at Imidazenil. It doesn't affect receptor density. I'm not so sure it would be helpful for our condition but it might prevent PAWS.
http://www.ncbi.nlm....les/PMC1909353/
I'll continue to post anything I find.
#93
Posted 16 September 2012 - 01:59 AM
They should have a drug that you take for a few weeks and in those weeks it will bring your GABA sites back to pre-benzo so in essence you should be back to 100% normality. I can tell you that the benzo withdrawal causes you to feel like a different person and your outlook on a normal day is as if you just landed from MARS
Edited by inw, 16 September 2012 - 02:00 AM.
#94
Posted 16 September 2012 - 02:33 AM
#95
Posted 16 September 2012 - 05:16 AM
#96
Posted 16 September 2012 - 06:45 AM
I'm not really depressed but feel lack of mental balance. Some anxiolysis would be welcomed too.
"Mechanism of Action of St John's Wort in Depression: What is Known?"
http://adisonline.co...1&type=abstract
Muira Puama is a natural GABA-A receptor antagonist. It could help with upregulation.
Edited by Galaxyshock, 16 September 2012 - 06:47 AM.
#97
Posted 16 September 2012 - 08:35 AM
I've been reading a bit about the pharmacology of the main 1st generation antihistamines that are OTC here (diphenhydramine, chlorphenamine and promethazine) and I see that theres a significant difference between them. Diphenhydramine has significant anticholinergic properties whereas promethazine doesn't. Promethazine won't cause the delirium that the OP described for diphenhydramine...
What I said in my previous reply was wrong. Promethazine does have moderate anticholinergic properties. I've never experienced any deliriant effects from it but I've never taken it in very high doses...
Mycotheologist,
Please kindly note that I am posting this with the desire to be HELPFUL to you (and others); so please kindly do not take it other than as it is intended.
I am not normally one for criticising other peoples' posts but, with the utmost respect, you need to ensure that your statements of 'fact' and advice to others are backed up by substantiated scientific evidence; as opposed to solely on what you have inferred from either your own singular personal self-administration / experimentation of a substance, which hence is merely a singular anecdotal report; or when your advice is based upon what you have inferred from "reading a bit about the pharmacology" wherein you have already demonstrated drawing conclusions that are wholly incorrect.
Please kindly note that I do not believe that I am never wrong, I can make mistakes just like everyone else; however, I most certainly ensure in all instances that my advice is properly substantiated by scientific evidence, and wherein the science is somewhat lacking, conflicting, insubstantial or anecdotal, I typically always will ensure that I state as such.
You need to start doing the same.
Suffice to say, by solely drawing upon your own personal singular anecdotal experience and what inferred from "reading a bit about the pharmacology" it is inevitable that some of your conclusions will be factually incorrect; and where you then go on to advise others the matter of SAFETY becomes a potential issue when we are dealing with substances that could be potentially harmful.
Take what you have posted about PROMETHAZINE for example... wherein PROMETHAZINE's primary mechanisms of action are ANTIHISTAMINE and ANTICHOLINERGIC; and yet you entirely incorrectly state "Diphenhydramine has significant anticholinergic properties whereas promethazine doesn't". Furthermore, the physician prescribing information for PROMETHAZINE warns about the possibility of EXCESSIVE ANTI-CHOLINERGIC EFFECTS, a.k.a. DELERIUM; and yet you again entirely incorrectly state "Promethazine won't cause the delirium that the OP described for diphenhydramine"... Do you see the problem? This could very well have resulted in someone, perhaps even the OP, taking PROMETHAZINE under the entirely false apprehension provided by your erroneous statements of fact and advice, and suffering an unpleasant and potentialy harmful adverse reaction... please be more careful
As I have already said, this sort of thing can easily be avoided by ensuring that all your future statements and advice is properly backed up by substantiated scientific evidence
I don't want to labour the point more than necessary, but suffice to say that you are guilty of doing precisely the same thing with regards to the following, wherein yet again you are wholly incorrect:
Don't take what ScienceGuy says as absolute truth. He has a lot of knowledge but we're all capable of being wrong about some things. Picamilon won't slow down your recovery too greatly. It is a GABA agonist though because GABA is the endogenous ligand for GABA receptors.
I feel the need to point out that we have previously in the past exchanges numerous messages via this forums PM system wherein I devoted a considerable amount of my personal time to helping you with your personally experiencing withdrawal from GABA RECEPTOR AGONISTS; including the fact that you mistakenly argued that PHENIBUT was not a GABAA RECEPTOR AGONIST, wherein I demonstrated to you that it most certainly is.
Further to this, it then became clear that you were under the misapprehension that switching between different substances would "avoid addiction" when in fact it transpires that all those substances are GABA RECEPTOR AGONISTS and hence your doing so was in fact part of the problem... To avoid continuing the same conversation in two different places I think it best if we continue it here where it is relevant to the topic of the thread; and as such to remind you, here is what you said and my reply:
I haven't been using GABAergics long enough to have incurred too many long lasting PAWs I don't think so I'm hoping I can make a full recovery using various supplements and time. I didn't have anxiety or insomnia before I started taking them, it was quite the opposite so that should make recovering a whole lot easier for me. I was only experimenting with them as sleep aids to counteract the dexedrine insomnia. Also, I only used benzos for a combined length of around 6 weeks, for the rest of that 6 month period I was experimenting with GHB, phenibut and z drugs (switching between these classes of drugs to avoid addiction).
In which case you have been taking GABA RECEPTOR AGONISTS consistently for "that 6 month period" and hence your GABA SYSTEM is most certainly to some extent DOWNREGULATEDThis is more or less unchartered territory though so I have no idea what the consequences will be when I completely quit. I quit for 3 weeks last month and taking my last dose of valium and while I could sleep every night, I had this anxious feeling the whole time.
This is totally expected given the existing partially DOWNREGULATED state of your GABA SYSTEM.
You already know what my advice is in this regard
In a nutshell, the reason that you have experienced (partial) relief from BENZODIAZEPINE WITHDRAWAL by taking other GABA RECEPTOR AGONISTS, including PICAMILION, is because they are activating THE SAME RECEPTORS; however, by doing so you will most certaining prolong your withdrawal. What you are doing is akin to treating HEROIN WITHDRAWAL by taking CODEINE. In short, usage of any and all GABA RECEPTOR AGONISTS should be tapered down and then stopped entirely
Downregulation of GABA_a receptors isn't necessarily the sole cause of protracted benzo w/d symptoms. In fact, I suspect its not even a significant part. I think Kompota is spot on. The problem is a structural change to the benzodiazepine site.
Suffice to say that this is yet another example of your making a statement without backing it up with any scientific substantiation; wherein said statement is based solely upon what you have inferred from either your own singular personal self-administration / experimentation of a substance, and hence is merely a singular anecdotal report; or when your advice is based upon what you have inferred from "reading a bit about the pharmacology".
Firstly, please kindly note that DOWNREGULATION OF GABA RECEPTORS in fact by definition includes STRUCTURAL CHANGES TO THE RECEPTOR SITES; so your entire statement is in fact a nonsense.
Secondly, there exists substantiated scientific evidence that demonstrates that DOWNREGULATION OF GABA RECEPTORS most certainly does play a primary role in BENZODIAZEPINE WITHDRAWAL.
See the following studies as just a couple of examples:
Lancet. 1982 Aug 14;2(8294):360-2.
Abstinence symptoms after withdrawal of tranquillising drugs: is there a common neurochemical mechanism?
Cowen PJ, Nutt DJ.
Abstract
Withdrawal of anxiolytic agents such as ethanol, barbiturates, and benzodiazepines may result in a syndrome characterised in its most severe form by delirium and seizures. There is increasing evidence that anxiolytic drugs produce their pharmacological effects by enhancing brain gamma-aminobutyric acid (GABA) transmission. During long-term exposure to anxiolytics [GABA Receptor Agonists], brain GABA synapses show evidence of adaptive changes which would tend to reduce the effect of the anxiolytic and restore normal GABA function. Abrupt cessation of anxiolytic treatment might therefore lead to an acute reduction in GABA function; this change could underlie the severe symptoms associated with tranquilliser withdrawal.
---------------------------------------------------------------------------------------------------------------------------
Neuropharmacology. 1982 Jan;21(1):85-9.
Chronic clonazepam administration induces benzodiazepine receptor subsensitivity.
Crawley JN, Marangos PJ, Stivers J, Goodwin FK.
Abstract
Clonazepam and chlordiazepoxide were administered chronically in increasing doses for three weeks in two different strains of mice. Forebrain [3H]diazepam binding was assayed in groups of mice sacrificed at 2, 26, 50 hr and 10 days following the last dose. Scatchard and single point analyses revealed a significant decrease in the number of [3H]diazepam binding sites [Bmax] which persisted for at least two days following chronic clonazepam treatment. The Bmax changes observed following chlordiazepoxide treatment were less pronounced than those elicited by clonazepam. No significant changes in receptor binding affinity (Kd)
were detected with either drug. In the clonazepam-treated animals, Bmax values returned to normal by day 10 after drug treatment. Chronic benzodiazepine administration therefore induced a decrease in the apparent number of benzodiazepine binding sites in the mouse forebrain. The magnitude and duration of the observed subsensitivity appears to depend on the potency of the administered benzodiazepine.
Edited by ScienceGuy, 16 September 2012 - 04:42 PM.
#98
Posted 16 September 2012 - 11:30 AM
ScienceGuy: I took alprazolam for exactly 1 week after quitting phenibut. Its been 2 days since my last dose of alprazolam and I'm back to normal. No withdrawal. I haven't even missed a nights sleep. On the 2nd day after stopping, I was depressed and anxious for the whole day but by nighttime, I felt fine. Now its day 3 and I feel good. I said it before and I'll say it again, phenibut exhibits VERY LOW cross tolerance with benzos so these 2 classes of drugs can be safely used to help circumvent each others acute withdrawal symptoms. Its nothing at all like treating an alcohol withdrawal with a few shots of vodka, its more like using gabapentin during an opioid withdrawal. I know you mean well but by following your advice to avoid ALL GABAergic drugs, people would be forcing themselves to endure completely unnecessary suffering. I've got off phenibut twice now with benzos and once with z drugs without needing to taper. This approach works. Theory is founded upon empirical observation, not the other way around. People need to know about this because it can save one a massive amount of suffering. I quit cold turkey from phenibut after a 2 week binge in the past and I couldn't sleep for 5 days straight and felt like crap for the duration of the withdrawal. This time I felt good the whole time.
I should mention though that while I feel fine if I take nothing, opioids give me real bad anxiety about 4 hours after I take them. Its interesting because I feel great for the first couple of hours then I gradually start getting more anxious. After reading a bit about opioid pharmacology I think I have a solid explanation. Opioids prevent GABA from being released so after I take them, my brain starts outputting less GABA and the levels of GABA in my brain gradually decrease. I've been taking dihydrocodeine which usually lasts around 6 hours and the anxiety is at its worst at around 6 hours. As the drug wears off, I start feeling good again as my GABA levels increase. Interesting stuff. I took some bacopa and gotu kola capsules but they didn't help at all. I didn't take any l-theanine so as not to further increase the amount of dopamine. I ordered some picamilon today so I'm looking forward to experimenting with it to see how it alleviates these mild protracted w/d symptoms.
Mycotheologist,
Salient points as follows:
1) RE: "Theory is founded upon empirical observation, not the other way around" - I feel the need to reiterate what I have said above, namely that you cannot and in fact must PLEASE STOP taking your your singular, non-placebo controlled, purely anecdotal experiences and wholly inappropriately, incorrectly and irresponsibly, without any scientific substantiation whatsoever, making statements and advising others as if medical fact.
If you have a THEORY that springs from personal OBSERVATION, you must not bipass the vital step of ascertaining whether or not there exists scientific evidence to support your THEORY, such as published studies etc.
Therefore, I strongly urge you to seek out said scientific evidence to confirm whether your THEORY has any validity, before posting your theories as if medical and/or scientific FACT.
This is what I typically do; so I am simply asking that you follow my example
2) I do not advise to "to avoid ALL GABAergic drugs" in the sense that you mistakenly infer, in that I clearly advise (as I have done with you previously) a TAPERING DOWN of use of all GABA RECEPTOR AGONISTS wherein one is treating someone for OVERUSE and/or ADDICTION to GABA RECEPTOR AGONISTS, which includes BENZODIAZEPINES.
3) I always strongly advise against 'STOPPING COLD TURKEY' due to the medically proven hazards associated with doing so.
4) Only once an appropriate TAPERING DOWN process has been completed should one cease and desist using GABA RECEPTOR, wherein one is advised to do so entirely, so as to prevent potential RELAPSE and reoccurrence of WITHDRAWAL SYMPTOMS.
5) You have never in fact ceased taking GABA RECEPTOR AGONISTS; you have simply switched randomly from one GABA RECEPTOR AGONIST to another wherein it is entirely unsurprising that you have attained temporary relief from your withdrawal symptoms, wherein it is precisely akin to "treating an alcohol withdrawal with a few shots of vodka".
This statement of yours says it all really:
I've got off phenibut twice now with benzos and once with z drugs without needing to taper. This approach works.... I felt good the whole time.
The fact of the matter is that PHENIBUT, BENZODIAZEPINES and Z-DRUGS are all GABA RECEPTOR AGONISTS, so you simply replaced one GABA RECEPTOR AGONIST (PHENIBUT) with another (BENZOS) in the first instance; and then replaced one GABA RECEPTOR AGONIST (PHENIBUT) with another (Z DRUGS) in the second instance... Wherein this is just one example of where you have never in fact ceased taking GABA RECEPTOR AGONISTS.
You have previously stated that PHENIBUT has no affinity for the GABAA RECEPTOR; wherein I subsequently demonstrated that it most certainly does.
You have ordered and repeatedly return to using PICAMILON; this also is a potent GABAA RECEPTOR AGONIST (a fact which should be obviously from its composition)
You have admitted also taking GHB, as well as Z-DRUGS, both of which are GABA RECEPTOR AGONISTS
You also have been and continue to experiment with taking other ADDICTIVE SUBSTANCES, including (but not limited to) OPIATES
I could go on...
My point is that you need to wake up and stop kidding yourself; you have a history of ADDICTION that includes ADDICTION to and WITHDRAWAL from GABA RECEPTOR AGONISTS; wherein, for the final time I will advise you to begin a proper and gradual TAPERING DOWN of any and all GABA RECEPTOR AGONISTS, at whatever rate / duration of time that keeps WITHDRAWAL SYMPTOMS to within tolerable range; and only once you have completed the TAPERING DOWN process, then cease your intake of any and all GABA RECEPTOR AGONISTS entirely.
There is no need to suffer unecessarily if one carries out the TAPERING DOWN process properly.
Think on this; the greatest step towards recovery is acknowledging that you have a problem.
I have considerable experience in treating ADDICTS and ADDICTION, so trust me I have seen and heard it all.
Incidentally, there is nothing wrong with your choosing to switch between taking PHENIBUT, BENZODIAZEPINES, Z-DRUGS, PICAMILON and other GABA RECEPTOR AGONISTS, so long as you recognise that you are in fact still taking GABA RECEPTOR AGONISTS
Furthermore, switching between multiple different GABA RECEPTOR AGONISTS is ill advised if one is carrying out a TAPERING DOWN process, for reasons which should hopefully be obvious
Finally, there are DRUGS and/or SUBSTANCES that can be highly useful in treating ADDICTION to and WITHDRAWAL from GABA RECEPTOR AGONISTS, whose mechanism(s) of action has nothing to do with AGONISM of the GABA RECEPTORS; regarding which I have already posted comprehensive information previously.
Edited by ScienceGuy, 16 September 2012 - 04:44 PM.
#99
Posted 16 September 2012 - 12:12 PM
ScienceGuy: ...You provide brilliant info but I think you have it wrong when say its best to steer clear of GABA_b agonists when recovering from GABA_a addiction. They allow you to safely and even comfortably get through acute withdrawal after quitting cold turkey...
Yeah but then you are just substituting one drug addiction for another whether they have cross tolerance or not...
Protoject,
Excellent point
Mycotheologist - you should listen to this fine gentleman, because he is absolutely correct
Firstly, as already mentioned PHENIBUT has affinity to both GABAB RECEPTORS (primary) and GABAA RECEPTORS (secondary); as such, if one completed the TAPERING DOWN and ceased taking GABAA RECEPTOR AGONISTS then it should be avoided.
Secondly, please kindly note that with regards to BACLOFEN, which is a SELECTIVE AGONIST of the GABAB RECEPTOR, one should not pay attention to the marketing spiel regarding it, since BACLOFEN is by no means a 'miracle drug' with regards to treating addiction, since it is now well established that it itself is ADDICTIVE and induces its own WITHDRAWAL SYMPTOMS; and hence I wholly concur with PROTOJECT, and for this reason alone taking GABAB RECEPTOR AGONISTS for treating WITHDRAWAL from GABAA RECEPTOR AGONISTS is not recommended, even if SELECTIVE for the GABAB RECEPTOR alone (wherein PHENIBUT and as it happens GHB are not).
See these studies for example:
Ann Fr Anesth Reanim. 1996;15(5):659-62.
Severe hyperthermia caused by sudden withdrawal of continuous intrathecal
administration of baclofen.
[Article in French]
Grenier B, Mesli A, Cales J, Castel JP, Maurette P.
Source
Département d'anesthésie-réanimation 3, hôpital Pellegrin, Bordeaux, France.
Abstract
Baclofen is used for the treatment of post-traumatic spasticity. It [Baclofen] carries a risk of overdose as well as of an acute withdrawal syndrome. We report two cases of severe hypertonia and hyperthermia (> 42 degrees C), occurring after accidental discontinuation of intrathecal infusion of baclofen. Both hypertonia and hyperthermia ceased when administration of baclofen was resumed. In parallel, the patients developed transient life-threatening alterations of hepatic (cytolysis), haematologic (coagulopathy) and cardiorespiratory functions for some days. It is concluded that the occurrence of such a withdrawal syndrome should be prevented, especially in patients with chronic intrathecal administration and first symptoms should be recognized without delay. Relationships with other malignant hyperthermias are discussed.
---------------------------------------------------------------------------------------------------------------------------
Psychosomatics. 2005 Nov-Dec;46(6):503-7.
Delirium associated with baclofen withdrawal: a review of common presentations and management strategies.
Leo RJ, Baer D.
Source
Department of Psychiatry, School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Erie County Medical Center, 462 Grider Street Buffalo, NY 14215, USA. rleomd@aol.com
Abstract
The authors reviewed 23 published cases of psychiatric symptoms in association with baclofen withdrawal. Delirium, and not other functional psychiatric conditions, arose secondarily from abrupt baclofen cessation. Vulnerability to baclofen-withdrawal delirium appeared to be greater in individuals who received chronic baclofen therapy. Baclofen-withdrawal delirium can be difficult to distinguish from elirium of other etiologies, and unrecognized and inadequately treated baclofen-withdrawal delirium is associated with significant morbidity and mortality. Complete resolution of delirium symptoms was possible with reinstatement of baclofen. The clinical management of patients experiencing baclofen-withdrawal delirium includes supportive interventions to reduce complications of delirium until symptoms resolve.
Edited by ScienceGuy, 16 September 2012 - 04:45 PM.
#100
Posted 16 September 2012 - 12:32 PM
I have no experience with this myself though. I think scienceguy is absolutely correct in that you should stay away from gaba agonists given that you taper down, which you didnt. Since you went cold turkey such a long time ago now you should be seeing light at the end of the tunnel, not feel worse. That makes no sense.
You may wish to take something with weak affinity for gabareceptors, something like theanine or such. And then taper that down (given it provides relief in the first place). Doubt you should start taking a benso again (for tapering down) as youve already made it so long without it...
Edited by Mikael, 16 September 2012 - 12:38 PM.
#101
Posted 16 September 2012 - 12:47 PM
Why did you quit cold turkey? For one its dangerous, as it can lead to convulsions. Secondly it causes a great deal of suffering.
Agreed
Usually a person switches to a benso with a LONG half-life and one that isnt very strong, not one with a short half-life as scienceguy claimed (in fact most of the bensos with short half-lifes have a much higher potential for addiction). Diazepam is usually the benso of choice due to ease of adminestration as well as a long half-life (ie tapering becomes easy and the risk for withdrawal symptoms coming on suddenly is minimized)
I clarified this point earlier; basically, it depends upon how far along the withdrawal / tapering down process you are as to whether LONG or SHORT HALF LIFE is recommended; please kindly read this:
Also, you say its best to use a short acting benzo to taper down. Its the other way around. You should use a long acting one like diazepam or clonazepam because longer acting benzos self taper and thus, give much milder withdrawals.
Sorry, I should have made this point more clearly. You are absolutely correct that the standard medical recommendation when commencing withdrawing from HIGH-POTENCY SHORT-ACTING BENZOS is to switch to a LONG-ACTING BENZO for the initial part of the tapering down process, with the intention of reducing the liklihood of rebound withdrawal symptoms occurring between doses. However, if one is in fact already quite a way down the road with regards to the tapering down process or if one is withhdrawing from taking either a MEDIUM or LONG ACTING BENZO then this phenomen is very unlike to occur; and in these cases it can in fact be most helpful to switch to a SHORT-ACTING BENZODIAZEPINE (preferably LOW-POTENCY) such that your GABA RECEPTORS are not hit 24/7 and hence can begin to recover...
#102
Posted 16 September 2012 - 12:52 PM
ScienceGuy, if you do not mind, I have some questions for you and I'll post them below.
1. So what is the goal here? From what I have read above, I need to avoid GABA agonists and try to take agents that upregulate GABAR?
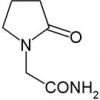
2. Why shouldn't I take Picamilon? It isn't a GABAR agonist per se. It provides the brain with more GABA (I do believe it crosses the BBB) but I would think that it is totally different than a GABAR agonist. Would it still cause downregulation? It will ignore the allosteric binding site and go right for the primary one.
3. What is your opinion of Afobazole? I am a little worried about its safety because it makes me nervous that it isn't widely used outside of Russia... Also, it is an MAOI. Does that mean I have to watch my tyramine intake when I take it?
4. Have you looked at Acamprosate for this condition? It would probably be useful for someone who is tapering off of benzos but would it help with someone with PAWS?
5. I know that time will help the most with this condition (hopefully it isn't permanent) but it could take years to feel appreciably better. Are there any other compounds you can think of that might help me rebalance my GABA receptors?
6. I've seen a couple of studies that found that Kava Kava is actually a GABAR upregulator. I'll post the thread.
http://www.longecity...250#entry535250
#103
Posted 16 September 2012 - 01:16 PM
Hello everyone,
WITHDRAWAL PROGRESS
My cold-turkey withdrawal has mostly abated. Looking back, I can share some information about how the supplements I tried affected the process.
I am really pleased to hear you are feeling better now, and my sympathies with regards to your suffering along the road to recovery. Thank you for posting this feedback which I am sure will be both helpful and interesting reading to others. A great thread quamquam91
Gotu kola gave me profound relief, but afterward my symptoms worsened. I believe that my sporadic use of gotu kola, holy basil, and other GABA-A agonists prolonged the overall process of withdrawing. They would clear up obsessive/fearful/repetitive thinking for a couple days, only to plunge me into a worsened schizoid state of mind after wearing off.
Very interesting... It is not unexpected to hear that "sporadic use of gotu kola, holy basil, and other GABA-A agonists prolonged the overall process of withdrawing"
I made my most grievous error two months ago. My symptoms had completely dispelled for a period of a few weeks, so I took the risk of drinking about three units of alcohol. Old withdrawal symptoms flared up, and I continue to suffer migraines, digestive problems, and brain fog that had previously cleared up.
Again, not unexpected. I guess you won't be making that "grievous error" again
SUPPLEMENT RETROSPECTIVE
In the thick of the withdrawal:
Inositol helped a great deal with anxiety without apparent ill effects when I stopped taking it. However, it seemed to worsen the tongue-tied feeling I had throughout withdrawal.
Bacopa flattened my mood and my thinking--I don't know how else to describe it. As with inositol, I had a harder time speaking fluently.
Piracetam seemed to help a bit, though combining it with choline was disturbing and dysphoric.
L-theanine was helpful. In large doses, profoundly flattening and asocial, and not good for sleep. (Made me feel like lying down, but did not assist me in falling asleep.) Pleasantly, combining l-theanine with caffeine helped me to do better socially, speak more clearly, and to think more sharply, while preventing the tweaked-out feeling that caffeine would usually cause while I was withdrawing.
Magnesium (either citrate or malate, which I tried on separate occasions) alleviated anxiety without having the flattening effect, but large doses caused my lymph nodes to swell up and turned my saliva into a sort of sour gel.
Fish oil affected me like speed while I was withdrawing. I think I took too much at once.
Decaffeinated coffee had a subtle soothing effect. It calmed my thinking and reduced unpleasant physical sensations (e.g. the feeling I would get that my skull was boiling from the inside--I am hyperbolizing, but you get the idea) with no discernible effect on my ability to fall asleep. I recommend decaf coffee above any other supplement I tried.
Thanks for the feedback! Did you try administering MAGNESIUM TRANSDERMALLY via soaking for >12 minutes within a hot bath into which 1-2 cups EPSOM SALTS (MAGNESIUM SULPHATE) has been dissolved? I wonder if you would experience the same unusual adverse effects if you were to do so. Perhaps worth trying?
BTW very interesting about the DECAFFEINATED COFFEE; just don't forget that DECAFFEINATED COFFEE is not in fact DECAFFEINATED, in that it still contains CAFFEINE, albeit a lot less
Edited by ScienceGuy, 16 September 2012 - 04:48 PM.
#104
Posted 16 September 2012 - 02:49 PM
Thank you for the tips! I know everyone is different and I see that it takes an average of 6-18 months to return to 100% pre benzo. Do you have any feedback on the timeframe it takes for the brain to return to homeostasis after being on benzos daily for a few years? I have people on for 3 months and it took 8-12 months for them to get back to normal.
#105
Posted 17 September 2012 - 12:14 AM
ScienceGuy, if you do not mind, I have some questions for you and I'll post them below.
Sorry for the delay in getting around to replying to your questions. I had read them in your earlier post, I wasn't ignoring you, but simply took a bit of time to catching up on replying to posts in this forum... too little time and too much to do and all that
1. So what is the goal here? From what I have read above, I need to avoid GABA agonists and try to take agents that upregulate GABAR?
Could you please kindly clarify exactly what it is that you are seeking to achieve and then (if possible without venturing off topic) I can offer my advice as to how best to achieve it
The "GOAL" of the OP was specifcally how best to move forward towards recovery from his/her existing situation of having (inadvisably) stopped taking BENZODIAZEPINES 'COLD TURKEY' wherein he was consequently experiencing a protracted POST ACUTE WITHDRAWAL SYNDROME (PAWS) for a prolonged period, complicated by intermittent usage of other GABA RECEPTOR AGONISTS etc...
I assume that your particular situation is not exactly the same as this?
2. Why shouldn't I take Picamilon? It isn't a GABAR agonist per se. It provides the brain with more GABA (I do believe it crosses the BBB) but I would think that it is totally different than a GABAR agonist. Would it still cause downregulation? It will ignore the allosteric binding site and go right for the primary one.
Firstly, please kindly note that I deliberately use the term GABA RECEPTOR AGONIST fairly loosely in my posts to facilate understanding and avoid confusion in readers who are not knowledgable in BIOCHEMISTRY.
Specifically, BENZODIAZEPINES are in fact POSITIVE ALLOSTERIC MODULATORS of the GABAA RECEPTOR, binding to the BENZODIAZEPINE RECEPTORS (which are in fact ALLOSTERIC MODULATORY SITES at the GABAA RECEPTOR); whereas GABA itself is a full GABAA RECEPTOR AGONIST and hence binds directly to the main receptor site at the GABAA RECEPTOR. Hence, PICAMILON (comprising GABA molecularly bonded to NIACIN) functions as a full GABAA RECEPTOR AGONIST and induces DOWNREGULATION of the GABAA RECEPTOR complex through ELEVATING CNS GABA LEVELS above normal.
Furthermore, GABAMIMETICS are proven to induce DOWNREGULATION of the GABA RECEPTORS and PICAMILION is a GABAMIMETIC
See the following for example:
Int Rev Neurobiol. 1996;39:53-76.
Use-dependent regulation of GABAA receptors.
Barnes EM Jr.
Source
Department of Biochemistry, Baylor College of Medicine, Houston, Texas 77030, USA.
Abstract
Prolonged occupancy of GABAA receptors by ligands, including GABA and benzodiazepine agonists, sets in motion a series of mechanisms that can be termed use-dependent regulation. These mechanisms can be subdivided into two distinct pathways, one for GABAA receptor downregulation and another for upregulation. Treatment of cortical neurons with GABA or benzodiazepines in cultures opens the pathway for GABAA receptor downregulation, which includes (in putative temporal order): (1) desensitization (tachyphylaxis), (2) sequestration (endocytosis) of subunit polypeptides and uncoupling of allosteric interactions between GABA and benzodiazepine binding sites, (3) subunit polypeptide degradation, and (4) repression of subunit gene expression. The end-point of GABAA receptor downregulation, a reduction in receptor number, is postulated to be established initially by degradation of the receptor protein and then maintained by a diminished level of de novo synthesis. Benzodiazepine treatment of many preparations, including cells expressing recombinant GABAA receptors, may elicit only desensitization, sequestration, or uncoupling, without a decline in receptor number. Components of the GABAA receptor downregulation pathway are also evoked by chronic administration of GABAmimetics, benzodiazepines, barbiturates, and neurosteroids in animals. This downregulation correlates with the establishment of tolerance to and physical dependence on the pharmacological effects of these drugs, suggesting a cellular model for this behavior.
3. What is your opinion of Afobazole? I am a little worried about its safety because it makes me nervous that it isn't widely used outside of Russia... Also, it is an MAOI. Does that mean I have to watch my tyramine intake when I take it?
You ask some excellent and very intelligent questions
Firstly, my current opinion on AFOBAZOLE is that it is a very interesting and potentially highly useful ANXIOLYTIC DRUG, because:
1) It does not in fact appear to have ANY direct interaction with the GABA RECEPTORS at all; wherein specifically its mechanism of action seems to be that of SIGMA AND MELATONIN RECEPTORS AGONIST and REVERSIBLE MAO-A INHIBITION;
2) It exerts both ANTIDEPRESSANT and ANXIOLYTIC with a reportedly good tolerability profile and without sedation, cognitive impairment or muscle relaxation, etc. and with demonstrated EFFICACY and SAFETY in preliminary human clinical trials.
That said, there currently exists a limited amount of published RESEARCH and/or STUDIES and as you say it isn't used widely outside of Russia, although this does not necessarily mean there are any issues with it.
With regards to it being an MAOI please kindly note that specifically it is a REVERSIBLE MAO INHIBITOR, and hence with regards to watching your dietary intake of TYRAMINE it is almost certainly the case that you would only need to avoid consumption of HIGH-TYRAMINE-CONTAINING CHEESES as this will be more than enough to prevent the risk of HYPERTENSIVE CRISIS. It is with regards to IRREVERSIBLE MAO INHIBITORS wherein dietary TYRAMINE intake becomes a problem
4. Have you looked at Acamprosate for this condition? It would probably be useful for someone who is tapering off of benzos but would it help with someone with PAWS?
ACAMPROSATE is a GABA RECEPTOR AGONIST with accompanying NMDA RECEPTOR ANTAGONIST mechanism of action; and as such indeed possibly useful for someone TAPERING OFF of BENZODIAZEPINES, but best avoided with PAWS
5. I know that time will help the most with this condition (hopefully it isn't permanent) but it could take years to feel appreciably better. Are there any other compounds you can think of that might help me rebalance my GABA receptors?
Mmmm... Yet another great question
The way I see it there exists two categories of substance that would prove helpful:
1) Substances that POSITIVELY influence the GABA SYSTEM;
Based on existing scientific evidence this would appear to include BACOPA MONNIERI, AFOBAZOLE and possibly THEANINE
If you are specifically treating POST ACUTE WITHDRAWAL SYNDROME (PAWS) due to BENZODIAZEPINE usage, then additionally, after (and only after) you have completed your TAPERING DOWN of any and all BENZODIAZEPINES, wherein you are no longer taking them (and they have left your system entirely), you might consider appropriate administration of a GABAA RECEPTOR ANTAGONIST that selectively acts at the BENZODIAZEPINE RECEPTOR SITE of the GABAA RECEPTOR, such as FLUMAZENIL.
This would effectively UPREGULATE your GABAA RECEPTORS, and specifically RE-SENSITIZE the BENZODIAZEPINE RECEPTOR SITE; wherein FLUMAZENIL's mechanism of action is akin to the mechanism of action of LOW DOSE NALTREXONE (LDN) therapy on UPREGULATING / RE-SENSITIZING the OPIATE RECEPTORS.
It is of course absolutely crucial that the FLUMAZENIL is administered properly, both with regards to ADMINISTRATION METHOD as well as DOSAGE; and furthermore, I must reiterate that it is imperative that administration of FLUMAZENIL is only commenced after you have ceased taking any and all BENZODIAZEPINES and they have left your system entirely (I can elaborate with regards to the details regarding why this is so important if you wish but this is already getting pretty technical and I don't want to overly confuse readers)
See the following EXTRACT FROM FULL TEXT from published study, wherein I have attached copies of the FULL TEXT for download:
J Psychopharma. 6(3) (1992) 357-363
A pilot study of the effects of flumazenil on symptoms persisting after benzodiazepine withdrawal
Malcolm H. Lader and Sally V. Morton
Source
Institute of psychiatry, De Crespigny Park, Denmark Hill, London SE5 8AF, UK
EXTRACT FROM FULL TEXT:
The potential of the benzodiazepine antagonist flumazenil (Ro 15-1788) to lessen persisting benzodiazepine withdrawal symptoms was demonstrated in 11 patients who had been drug free for between 1 month and 5 years. Doses ranging from 0.2 to 2.0 mg divided into three intravenous injections over a few hours relieved long-standing symptoms to varying extents. These included clouded thinking, tiredness, muscular symptoms such as neck tension, cramps and shaking and the characteristic perceptual symptoms of benzodiazepine withdrawal, namely, pins and needles, burning skin, pain and subjective sensations of bodily distortion. Mood disorder, when present, also improved but the reduction in anxiety and depression may have reflected relief of physical symptoms. The onset of maximum response was sometimes delayed by as much as a day but was usually prompt.
Side effects were reported to be either absent or typically described as lightheadedness or dizziness, lasted only a few minutes and were usually well tolerated.
The benefits last between a few hours and several days despite flumazenil's otherwise short duration of action.
However, symptoms did return to varying degrees in most cases, suggesting the need for repeated doses.
Discussion
Our impression from this, our first experience in patients, is that the benzodiazepine antagonist flumazenil does have potential to treat persisting benzodiazepine withdrawal symptoms. To varying degrees, sometimes dramatically, it reduced both physical and mental symptoms which had persisted for months or even years after withdrawal. Musculo-perceptual symptoms such as muscle tension, spasms, shakes and burning halved in intensity…
As we were experimenting with a non-licensed indication, we exercised the utmost caution in the first patients using only 0.5 mg. However, later patients easily tolerated the higher dose of 2.0 mg.
-------------------------------------------------------------------------------------------------------------------------------------------
RE: ADMINISTRATION METHOD - Please note that FLUMAZENIL cannot be taken PER ORALLY due to poor absorption, and it is typically administered via INTRAVENOUS INJECTION; which would make it somewhat impractical / unfeasible for the general population to administer. However, the good news is that FLUMAZENIL can quite simply be administered INTRANASALLY. See the following study that demonstrates this:
Can J Anaesth. 2000 Feb;47(2):120-4.
Plasma concentration of flumazenil following intranasal administration in children.
Scheepers LD, Montgomery CJ, Kinahan AM, Dunn GS, Bourne RA, McCormack JP.
Source
Department of Anesthesia, University of British Columbia, Vancouver, Canada. louissch@home.iatronet.net
Abstract
PURPOSE:
A pharmacokinetic study in children to determine plasma flumazenil concentrations after the intranasal administration of 40 microg x kg(-1).
METHODS:
Following institutional approval and informed written consent, 11 ASA physical status I-II patients, aged two to six years, undergoing general anesthesia for dental surgery were recruited. After induction, 40 microg x kg(-1) flumazenil Anexate, Roche, 0.1 mg x mL(-1) (0.4 mL x kg(-1))) were administered via a syringe as drops, prior to nasal intubation. Venous plasma samples were drawn prior to administration of flumazenil (t = 0), and then at 2, 4, 6, 8, 10, 15, 20, 30, 40, 60, and 120 min thereafter. The plasma samples were immediately processed by the on-site laboratory and then stored at -70 degrees C, before batch analysis via high performance liquid chromatography assay. Pharmacokinetic data calculations were performed using WinNonLin software (Scientific Consulting Inc.).
RESULTS:
Eleven patients were studied, but data for one patient were discarded due to insufficient sampling. The median age was 4.3 yr (range 3 to 6), with a median weight of 18.9 kg (range 14.9 to 22.2). There were seven boys and three girls. Mean Cmax was 67.8 ng x mL(-1) (SD 41.9), with Tmax at two minutes. The calculated half-life was 122 min (SD 99).
CONCLUSION:
The mean plasma concentrations of flumazenil attained [after intranasal administration] were similar to those reported after intravenous administration, and may be sufficient to antagonize the side-effects of benzodiazepines. This route of administration may be useful when the intravenous route is not readily available.
-------------------------------------------------------------------------------------------------------------------------------------------
2) Substances that effectively treat the SYMPTOMATOLOGY associated with PAWS without NEGATIVELY influencing the GABA SYSTEM.
This is where the likes of NMDA RECEPTOR ANTAGONISTS such as MAGNESIUM and other substances that fall within this remit would be helpful
6. I've seen a couple of studies that found that Kava Kava is actually a GABAR upregulator. I'll post the thread.
http://www.longecity...250#entry535250
See what I have posted in that thread: Kava Kava for Anxiolysis and GABA-a Receptor Upregulation
In short, there currently exists CONFLICTING scientific evidence regarding that
Attached Files
Edited by ScienceGuy, 17 September 2012 - 12:26 AM.
#106
Posted 17 September 2012 - 12:22 AM
Don't take what ScienceGuy says as absolute truth. He has a lot of knowledge but we're all capable of being wrong about some things... Downregulation of GABA_a receptors isn't necessarily the sole cause of protracted benzo w/d symptoms. In fact, I suspect its not even a significant part... That would explain why flumazenil produces long lasting relief from protracted withdrawal symptoms. Flumazenil is an inverse BZ agonist so its the polar opposite of a benzo.
Heres a few GABA_a inverse agonists...
Very interesting, yea it sucks that all of these Benzo 'reversable' drugs are not OTC...
OK, firstly please can we kindly dispense with the "inverse BZ agonist" and "Benzo reversible drugs" milarkey
FLUMAZENIL is a GABAA RECEPTOR ANTAGONIST that acts selectively at the BENZODIAZEPINE RECEPTOR SITE at the GABAA RECEPTOR.
Furthermore, the reason why FLUMAZENIL "produces long lasting relief from protracted withdrawal symptoms" is due to UPREGULATING the GABAA RECEPTORS and specifically RE-SENSITIZING the BENZODIAZEPINE RECEPTOR SITE at the GABAA RECEPTOR.
Hence, DOWNREGULATION of the GABA RECEPTORS most certainly is "a significant part" of the "cause of protracted benzo w/d symptoms"
#107
Posted 17 September 2012 - 01:10 AM
ScienceGuy
Thank you for the tips! I know everyone is different and I see that it takes an average of 6-18 months to return to 100% pre benzo. Do you have any feedback on the timeframe it takes for the brain to return to homeostasis after being on benzos daily for a few years? I have people on for 3 months and it took 8-12 months for them to get back to normal.
The time taken for status to return entirely to baseline would depend upon a considerable number of factors, so it is unfortunately impossible to provide a singular answer to your question
The 'bad news' is that you are indeed correct that there are indeed instances wherein prolonged persistent usage of BENZODIAZEPINES for a number of months can take many months to fully recover; however, the 'good news' is that this is almost always wherein no countermeasures are implimented to accelerate the recovery process and/or the situation is prolonged through inadvertently taking substances that are unhelpful in such situations.
By employing a proper TAPERING OFF of BENZODIAZEPINES, combined with appropriate measures to promote recovery of your GABA RECEPTOR FUNCTION, and avoid further DOWN-REGULATION of the GABA RECEPTORS, would significantly accelerate the normal recovery time.
#108
Posted 17 September 2012 - 04:22 AM
ScienceGuy
Thank you for the tips! I know everyone is different and I see that it takes an average of 6-18 months to return to 100% pre benzo. Do you have any feedback on the timeframe it takes for the brain to return to homeostasis after being on benzos daily for a few years? I have people on for 3 months and it took 8-12 months for them to get back to normal.
The time taken for status to return entirely to baseline would depend upon a considerable number of factors, so it is unfortunately impossible to provide a singular answer to your question
The 'bad news' is that you are indeed correct that there are indeed instances wherein prolonged persistent usage of BENZODIAZEPINES for a number of months can take many months to fully recover; however, the 'good news' is that this is almost always wherein no countermeasures are implimented to accelerate the recovery process and/or the situation is prolonged through inadvertently taking substances that are unhelpful in such situations.
By employing a proper TAPERING OFF of BENZODIAZEPINES, combined with appropriate measures to promote recovery of your GABA RECEPTOR FUNCTION, and avoid further DOWN-REGULATION of the GABA RECEPTORS, would significantly accelerate the normal recovery time.
Thanks once again for the response. I tapered very slowly under the dr's plan (tapered from 3mg xanax per day to .25mg over 2 years). I was taking celexa at the time too. It seems after a month of the .25mg I hit tolerance withdrawal, high anxiety, extreme lethargy, mood was depressed, etc.. Then a few more months of tapering I finished the celexa and then the xanax. I'm 4 months and 2 weeks off the xanax now.
My questions are:
1) Do the GABA receptors ONLY start to heal after you discontinue the benzo?
2) OR dot he GABA receptors start getting back to normal during your slow taper?
My feedback
It really seems like if you are prone to the withdrawal it will happen no matter what once you finish your last dose. Some people have no issues during their taper but a few weeks after their last dose, the withdrawal starts. That is why I am wondering when the healing really starts.
#109
Posted 18 September 2012 - 07:33 PM
----------
"Sorry for the delay in getting around to replying to your questions. I had read them in your earlier post, I wasn't ignoring you, but simply took a bit of time to catching up on replying to posts in this forum... too little time and too much to do and all that
Haha I figured. No problem at all. I appreciate you answering my 3190839403184903 questions.
----------
"Could you please kindly clarify exactly what it is that you are seeking to achieve and then (if possible without venturing off topic) I can offer my advice as to how best to achieve it
I also suffer from benzo PAWS as you probably know by now. I just want to get better as soon as possible.
----------
"Treatment of cortical neurons with GABA or benzodiazepines in cultures opens the pathway for GABAA receptor downregulation, which includes (in putative temporal order): (1) desensitization (tachyphylaxis), (2) sequestration (endocytosis) of subunit polypeptides and uncoupling of allosteric interactions between GABA and benzodiazepine binding sites, (3) subunit polypeptide degradation, and (4) repression of subunit gene expression."
My best guess is that tachyphylaxis to benzodiazepines leads to initial withdrawal symptoms after cessation (I never used them frequently enough to get withdrawal) and PAWS is caused by the uncoupling of allosteric interactions between GABA and benzodiazepine binding. But I have never heard of anyone getting PAWS from taking GABA supplements or other positive allosteric modulators (assuming of course that these individuals have never taken benzodiazepines). It seems as if the uncoupling of those interactions is the body's "defense mechanism" that it employs to try to get back to homeostasis. It's all very interesting stuff.
----------
"...Wherein FLUMAZENIL's mechanism of action is akin to the mechanism of action of LOW DOSE NALTREXONE (LDN) therapy on UPREGULATING / RE-SENSITIZING the OPIATE RECEPTORS.
I have a study here (I'll post below) that found that naloxone administration antagonizes and consequently upregulates GABA receptors... The full text is available on that same page. What are your thoughts on that? I could probably convince my doctor to give me some...
http://www.springerl...bux9vblgf7rn4f/
Abstract
Several lines of behavioral and neurochemical evidence indicate GABAA-antagonistic properties of naloxone. Here, the effects of naloxone on rat brain GABAA/benzodiazepine receptor function in vitro were investigated. Naloxone, naltrexone and morphine (10–1,000 μM) reduced GABA-induced (10 μM) 36Cl− uptake in corticohippocampal synaptoneurosomes. Furthermore, the concentration-response curve for GABA-induced 36Cl− uptake (GABA 3–100 μM) was shifted to the right both by naloxone and morphine (1,000 μM). Naloxone also reduced the 36Cl− uptake induced by GABA + diazepam (3 μM + 1 μM) but not that induced by amobarbital (500 μM). The naloxone-induced (1,000 μM) reduction of GABA-mediated (10 μM) 36Cl− uptake was reversed by amobarbital (10–1,000 μM) but not by flumazenil (10–1,000 μM) or morphine (0.1–1,000 μM). These results indicate that naloxone, naltrexone and morphine are weak negative modulators of GABAA/benzodiazepine receptor function. The naloxone effect most likely does not involve opiate receptors or the benzodiazepine site on GABAA receptor complexes.
----------
"This is where the likes of NMDA RECEPTOR ANTAGONISTS such as MAGNESIUM and other substances that fall within this remit would be helpful
Yeah I am going to start taking Theanine, Bacopa, and possibly Afobazole. So does this mean that an NMDA antagonist like Memantine might be helpful? If so, do you think it would actually upregulate the GABAergic system and speed the process of recovery? I'm thinking that at the very least, it will help with some of my PAWS symptoms. I could definitely get this from my Psychiatrist if I made a good argument and presented plenty of relevant studies to him.
And while we're on the topic of NMDA receptors... would it be a bad idea to activate the glutamatergic system in people with PAWS? I'm thinking specifically of the racetams... I'm also wondering what the effect would be if I combined Memantine and a racetam...
----------
I realize this is a lot to digest. Take your time in responding.
#110
Posted 18 September 2012 - 08:13 PM
ScienceGuy: ...You provide brilliant info but I think you have it wrong when say its best to steer clear of GABA_b agonists when recovering from GABA_a addiction. They allow you to safely and even comfortably get through acute withdrawal after quitting cold turkey...
Yeah but then you are just substituting one drug addiction for another whether they have cross tolerance or not...
Protoject,
Excellent point
Mycotheologist - you should listen to this fine gentleman, because he is absolutely correct
This is the very thing I am talking about. Myself and countless others have successfully circumvented phenibut withdrawal by using selective GABA_a agonists such as benzos or barbiturates. It is NOT substituting one addiction for another. It is NOT like replacing a heroin addiction with a morphine addiction. Heroin is a non selective opioid agonist that acts on mu, delta and kappa receptors. The situation is more akin to using deltorphin (a selective delta opioid agonist) to remedy symptoms of addiction to a selective mu opioid agonist. If one quits phenibut cold turkey, they won't sleep for at least 5 days and have various withdrawal symptoms. If on the other hand, one takes a benzo for 2 weeks after quitting phenibut cold turkey, they will experience no insomnia or significant w/d symptoms after stopping the benzo. I can't back this up with a scientific study because there has never been a study done on this. This is my personal experience and there are plenty of anecdotal reports backing this up. Lack of evidence in support of something does not constitute evidence contrary to it.
As for what I said about promethazine, yeah I was wrong. I corrected myself directly afterwards. While you're right that one should back up what they say with scientific articles when they're available, sometimes all that exists is anecdotal evidence as no scientific studies have been performed investigating a particular area, as is the case with using a benzo during phenibut withdrawal. Heres an article on flumazenil:
http://www.bcnc.org.uk/flumazenil.html
As I said, its unknown the exact cause of protracted benzo withdrawal symptoms. You can't back your claim that GABAR downregulation are a significant factor up with scientific evidence because none exists.An alternative explanation is that chronic agonist use causes a persistent conformational change and thus a shift in benzodiazepine receptor efficacy in the direction of inverse agonist function (Little, Nutt and Taylor, 1987) and that flumazenil resets the receptor's sensitivity (Nutt and Costello, 1988). In binding to the benzodiazepine receptor flumazenil may alter the coupling of the elements of the GABA/benzodiazepine macromolecular complex modified by benzodiazepine binding, thus restoring the GABA recognition site to its pre-drug affinity (Gonsalves and Gallager, 1985).
EDIT: I just came across this webpage:
http://web.squ.edu.o...2/020251r00.htm
heres a quote from it:
if thats correct, then you're right. The mechanism behind the long lasting relief can't be due to it inversely agonising the BZ receptor site. It also seems to contradict the theory that flumazenil provides relief by antagonising an endogenous BZ inverse agonist because if that were the case, flumazenil would actually increase GABA activity. Unless there are also endogenous BZ agonists present, which are present in much lower concentrations during BZ withdrawaal.When given in the absence of a benzodiazepine receptor agonist, flumazenil has little discernible CNS effect. Although intrinsic (agonist and inverse agonist) effects have been ascribed to flumazenil, 85 they are clinically unimportant. It has been postulated that in low doses a stimulating effect can be seen, and in high doses a central depressant effect becomes more likely.
You have vastly greater knowledge of pharmacology than I do, I merely said that not everything you say is necessarily accurate, which in my experience is the case with what you say about benzodiazepines being ineffective in treating a phenibut withdrawal. I can say with absolute certainty that the approach works. I have used it to circumvent 3 phenibut withdrawals so far.
Edited by mycotheologist, 18 September 2012 - 09:13 PM.
#111
Posted 18 September 2012 - 09:22 PM
Trazodone behaves as an antagonist at all of the following receptors except 5-HT1A where it acts as a partial agonist similarly to buspirone and tandospirone but with greater intrinsic activity in comparison:[18][19][20][21][22][23]
- 5-HT1A receptor (Kd = 78 nM)
- 5-HT2A receptor (Ki = 13 nM)
- 5-HT2B receptor (Ki = 74 nM)[24]
- 5-HT2C receptor (Ki = 192 nM)
- α1-adrenergic receptor (Kd = 39 nM)
- α2-adrenergic receptor (Kd = 405 nM)
- H1 receptor (Kd = 725 nM)
- SERT (Kd = 160 nM)
#112
Posted 19 September 2012 - 04:25 PM
http://www.ncbi.nlm....pubmed/18492727
Burning of Boswellia resin as incense has been part of religious and cultural ceremonies for millennia and is believed to contribute to the spiritual exaltation associated with such events. Transient receptor potential vanilloid (TRPV) 3 is an ion channel implicated in the perception of warmth in the skin. TRPV3 mRNA has also been found in neurons throughout the brain; however, the role of TRPV3 channels there remains unknown. Here we show that incensole acetate (IA), a Boswellia resin constituent, is a potent TRPV3 agonist that causes anxiolytic-like and antidepressive-like behavioral effects in wild-type (WT) mice with concomitant changes in c-Fos activation in the brain. These behavioral effects were not noted in TRPV3(-/-) mice, suggesting that they are mediated via TRPV3 channels. IA activated TRPV3 channels stably expressed in HEK293 cells and in keratinocytes from TRPV3(+/+) mice. It had no effect on keratinocytes from TRPV3(-/-) mice and showed modest or no effect on TRPV1, TRPV2, and TRPV4, as well as on 24 other receptors, ion channels, and transport proteins. Our results imply that TRPV3 channels in the brain may play a role in emotional regulation. Furthermore, the biochemical and pharmacological effects of IA may provide a biological basis for deeply rooted cultural and religious traditions.
Heres a sciencedaily article on it:
http://www.scienceda...80520110415.htm
That single abstract isn't much to go on but its worth looking into in my opinion. I tried smoking frankincense resin and its harsh on the throat but if sitting in a room with burning frankincense is enough to cause a mood change, then one wouldn't need to smoke much. I don't really have any significant remaining w/d symptoms to test this out on at the moment but if I get a wave of anxiety/depression, I'm going to test it out. Not suggesting anyone else do this as there may be harmful compounds in the smoke but I don't mind being a guinea pig for this.
Edited by mycotheologist, 19 September 2012 - 04:30 PM.
#113
Posted 19 September 2012 - 04:43 PM
Secondly, there exists substantiated scientific evidence that demonstrates that DOWNREGULATION OF GABA RECEPTORS most certainly does play a primary role in BENZODIAZEPINE WITHDRAWAL.
See the following studies as just a couple of examples:
Lancet. 1982 Aug 14;2(8294):360-2.
Abstinence symptoms after withdrawal of tranquillising drugs: is there a common neurochemical mechanism?
Cowen PJ, Nutt DJ.
Abstract
Withdrawal of anxiolytic agents such as ethanol, barbiturates, and benzodiazepines may result in a syndrome characterised in its most severe form by delirium and seizures. There is increasing evidence that anxiolytic drugs produce their pharmacological effects by enhancing brain gamma-aminobutyric acid (GABA) transmission. During long-term exposure to anxiolytics [GABA Receptor Agonists], brain GABA synapses show evidence of adaptive changes which would tend to reduce the effect of the anxiolytic and restore normal GABA function. Abrupt cessation of anxiolytic treatment might therefore lead to an acute reduction in GABA function; this change could underlie the severe symptoms associated with tranquilliser withdrawal.
---------------------------------------------------------------------------------------------------------------------------
Neuropharmacology. 1982 Jan;21(1):85-9.
Chronic clonazepam administration induces benzodiazepine receptor subsensitivity.
Crawley JN, Marangos PJ, Stivers J, Goodwin FK.
Abstract
Clonazepam and chlordiazepoxide were administered chronically in increasing doses for three weeks in two different strains of mice. Forebrain [3H]diazepam binding was assayed in groups of mice sacrificed at 2, 26, 50 hr and 10 days following the last dose. Scatchard and single point analyses revealed a significant decrease in the number of [3H]diazepam binding sites [Bmax] which persisted for at least two days following chronic clonazepam treatment. The Bmax changes observed following chlordiazepoxide treatment were less pronounced than those elicited by clonazepam. No significant changes in receptor binding affinity (Kd)
were detected with either drug. In the clonazepam-treated animals, Bmax values returned to normal by day 10 after drug treatment. Chronic benzodiazepine administration therefore induced a decrease in the apparent number of benzodiazepine binding sites in the mouse forebrain. The magnitude and duration of the observed subsensitivity appears to depend on the potency of the administered benzodiazepine.
I briefly skimmed through your posts yesterday but I'm reading them in more detail now. Be careful not to misinterpret abstracts. The first abstract states that there is a decrease in GABA function, it does not state the cause of this decrease in GABA function. It could be downregulation of GABA_a receptors, but it could also be that the benzodiazepine or barbiturate binding sites adopt an inverse agonist conformation, forcing the active site of the receptor into a less active conformation, which GABA has less affinity for.
The second abstract states that repeated benzo use induces a decrease in "the apparent number of benzodiazepine binding sites". Apparent is a keyword there (meaning they don't know whether there is actually a decrease in the number of BZ sites, but rather they are speculating based on the observed decrease in GABA function) but besides that, cells can downregulate the BZ receptor site itself, rather than downregulating the actual GABA_a receptor.
Mycotheologist,
Salient points as follows:
1) RE: "Theory is founded upon empirical observation, not the other way around" - I feel the need to reiterate what I have said above, namely that you cannot and in fact must PLEASE STOP taking your your singular, non-placebo controlled, purely anecdotal experiences and wholly inappropriately, incorrectly and irresponsibly, without any scientific substantiation whatsoever, making statements and advising others as if medical fact.
If you have a THEORY that springs from personal OBSERVATION, you must not bipass the vital step of ascertaining whether or not there exists scientific evidence to support your THEORY, such as published studies etc.
Therefore, I strongly urge you to seek out said scientific evidence to confirm whether your THEORY has any validity, before posting your theories as if medical and/or scientific FACT.
If everyone followed this line of thought, then the knowledge of ibogaines anti-addictive properties would not be known today. It was discovered accidentally by a junkie who took it to get high one day. If he had just thought "there are have not been any scientific studies done on ibogaines use as an addiction interrupter so I wont tell anyone about my discovery" we may not (probably not) know about ibogaines anti-addictive properties today. Like I said, theory is founded on empirical observation, not the other way around. Just because there have been no scientific studies done which support an observation, does not make the observation any less valid. A vast amount of pharmaceutical compounds in use today, were discovered as a result of anecdotal knowledge. An example is curare. The indigenous people who developed this complex mixture of compounds knew it worked from observation. Eventually scientists took notice and studied the substance and discovered that it paralyses the nervous system by blocking nicotinic ACh receptors at the neuromuscular junction. Like I said, scientific theory is founded upon empirical observation, not the other way around. Maybe pharmacologists will decide to do a double blind study investigating the potential use of selective GABA_b agonists to treat benzo withdrawal or vice versa, but until then all we have is anecdotal evidence. This thread isn't the place for us to debate our views though, so lets just agree to disagree.
Edited by mycotheologist, 19 September 2012 - 05:06 PM.
#114
Posted 19 September 2012 - 05:20 PM
I can't help it, I have to respond to your posts. Despite them having a common ligand, GABA_a and GABA_b are two completely different receptors. One is a ligand gated chloride channel, the other is a metabotropic receptor.The fact of the matter is that PHENIBUT, BENZODIAZEPINES and Z-DRUGS are all GABA RECEPTOR AGONISTS, so you simply replaced one GABA RECEPTOR AGONIST (PHENIBUT) with another (BENZOS) in the first instance; and then replaced one GABA RECEPTOR AGONIST (PHENIBUT) with another (Z DRUGS) in the second instance... Wherein this is just one example of where you have never in fact ceased taking GABA RECEPTOR AGONISTS.
You didn't demonstrate anything, you simply quoted an article.You have previously stated that PHENIBUT has no affinity for the GABAA RECEPTOR; wherein I subsequently demonstrated that it most certainly does.
http://onlinelibrary...0211.x/abstract
this article would suggest it has low and potentially insignificant GABA_a activity. Heres a quote from wikipedia:Phenibut (β-phenyl-γ-aminobutyric acid HCl) is a neuropsychotropic drug that was discovered and introduced into clinical practice in Russia in the 1960s. It has anxiolytic and nootropic (cognition enhancing) effects. It acts as a GABA-mimetic, primarily at GABAB and, to some extent, at GABAA receptors. It also stimulates dopamine receptors and antagonizes β-phenethylamine (PEA), a putative endogenous anxiogenic. The psychopharmacological activity of phenibut is similar to that of baclofen, a p-Cl-derivative of phenibut. This article reviews the structure-activity relationship of phenibut and its derivatives. Emphasis is placed on the importance of the position of the phenyl ring, the role of the carboxyl group, and the activity of optical isomers. Comparison of phenibut with piracetam and diazepam reveals similarities and differences in their pharmacological and clinical effects. Phenibut is widely used in Russia to relieve tension, anxiety, and fear, to improve sleep in psychosomatic or neurotic patients; as well as a pre- or post-operative medication. It is also used in the therapy of disorders characterized by asthenia and depression, as well as in post-traumatic stress, stuttering and vestibular disorders.
I already quoted from reference 1, heres the full article:There is dispute in the literature about whether or not Phenibut binds to the GABAA ionotropic receptor, which is responsible for the actions of the benzodiazepines, barbiturates, z-drugs, and for some of the effects of ethanol. According to Allikmetz and Ryage (1983) and Shulgina (1986) phenibut does bind to the GABAA receptor,[2] but according to Lapin (2001) it does not.[1] In the case of the former, it is argued that the GABAA binding only occurs at higher concentrations.[2]
http://onlinelibrary...1.tb00211.x/pdf
heres reference 2:
https://www.ncbi.nlm.../pubmed/2431377
I couldn't get the full article with my university account for some reason.
thegrons right so I'll shut up now unless I have some useful info to add.
Edited by mycotheologist, 19 September 2012 - 05:47 PM.
#115
Posted 19 September 2012 - 06:29 PM
Sixty (60) out-patients with DSM III generalized anxiety disorder were treated after a 1-week placebo washout in a 4-week double-blind study with buspirone, diazepam and placebo; after which they were withdrawn abruptly from medication or assigned to a 2-week period of placebo. The HAM-A score was significantly lower in the diazepam group at week 2 (p less than .02) and the buspirone group at week 3 (p less than .04) as compared to the placebo group. A similar pattern was evident in the female group, but not in the male group. Dizziness was the most prominent adverse effect in the buspirone group, whereas the diazepam group had more adverse effects including sedation, fatigue, dizziness and impaired concentration. Withdrawal symptoms were more evident in the diazepam group than the buspirone group.
Heres a compound with a completely novel mechanism of action:
www.bionomics.com.au/siteFiles/files/ECNP%20CCK%20Poster-4.pdf
but I don't know if one can obtain it. Maybe it can be ordered from chemical suppliers.BNC210 is a novel compound in development for the treatment of Generalized Anxiety Disorder (GAD) with co-morbid depression. It
exhibits potent anxiolytic and antidepressant activity in preclinical animal models without displaying the side effects of currently marketed
treatments for anxiety (benzodiazepines and SSRIs). BNC210 has a particularly strong anxiolytic effect in rodent models of physically
induced stress (e.g., forced swim stress followed by Elevated Plus-maze (EPM)), which has led to its evaluation in a rodent model of
pharmacologically induced stress.
Cholecystokinin (CCK) is a neurotransmitter, hormone and neuromodulator which binds to CCKA and CCKB receptors. Two centrally active
peptides of CCK, the tetrapeptide CCK-4 and the unsulfated octapeptide CCK-8us, have a high affinity for CCKB receptors which are
distributed widely throughout the brain. The involvement of CCK in human anxiety is well documented and the administration of CCKB
receptor agonists such as CCK-4, provokes panic attacks in man and provides a model for assessing novel anxiolytic compounds in healthy
volunteers. BNC210 has been evaluated in Phase I trials for safety, tolerability and food effect (See poster P.4.a.010).
I just found this article which is interesting:
http://www.ncbi.nlm....pubmed/19394358
My doc prescribed me tablets containing 500mg amoxicillin and 125mg clavulanic acid, I have a few left over so I'll test them out next time I get a wave of anxiety.Clavulanic acid is a member of the beta lactam family of antibiotics with little or no intrinsic antibacterial activity of its own; instead, it is used to enhance the activity of antibiotics by blocking bacterial beta-lactamases. Because clavulanic acid by itself is very safe, orally active and shows good brain penetrance, we sought to determine if it had any potential as a psychotherapeutic. Clavulanic acid was a tested across three mammalian species, hamsters, rats and cotton-top tamarin monkeys in a series of behavioral assays designed to screen for anxiolytic activity. In addition, several studies were done in rodents to compare the behavioral profile of clavulanic acid to the commonly prescribed benzodiazepines, particularly with respect to their unwanted side effects of motor depression, amnesia and neuroendocrine dysregulation.
Our findings show that clavulanic acid is a highly potent anxiolytic in rodents without altering motor activity in the open field test, normal learning and memory in the Morris water maze, or normal stress hormone release. Orally administered clavulanic acid significantly reduces measures of anxiety in male/female pairs of cotton-top tamarins. In addition, male tamarins showed a highly significant increase in sexual arousal as measured by the number of penile erections. The fact clavulanic acid has anxiolytic activity in the tamarin holds the promise that this drug may be an effective therapeutic for the treatment of anxiety disorders in humans.
Edited by mycotheologist, 19 September 2012 - 07:04 PM.
#116
Posted 19 September 2012 - 06:41 PM
#117
Posted 19 September 2012 - 07:19 PM
Two more classes of anxiolytics that I'm reading about are CCK-B antagonists and CRF antagonists.
http://www.ncbi.nlm....icles/PMC54610/
Development of a class of selective cholecystokinin type B receptor antagonists having potent anxiolytic activity.
PD134308 and PD135158 are potent and selective antagonists at the cholecystokinin type B (CCK-B) receptors with IC50 values of 1.6 nM and 3.5 nM, respectively, in the radioligand binding assay and Ke values of 7.82 and 12.9 nM, respectively, in their blocking action on CCK responses in the rat lateral hypothalamic slice. PD134308 and PD135158 produced potent anxiolytic effects in the mouse black/white box test after either subcutaneous or oral administration. There was no evidence of the development of tolerance to the anxiolytic action of either PD134308 or PD135158 in mice treated twice daily for 7 days, nor was there any sign of withdrawal anxiogenesis after abrupt termination of this treatment. Both CCK-B antagonists were able to suppress the withdrawal anxiogenesis and produce an anxiolytic effect in mice previously made tolerant to diazepam. PD134308 and PD135158 produced potent anxiolytic effects in the rat elevated plus maze test and the rat social interaction test. The effects were comparable in magnitude to those seen with diazepam. However, unlike diazepam, PD134308 and PD135158 did not produce sedation. The CCK-B antagonists also showed powerful anxiolytic activity in the "marmoset human threat test." These results provide evidence of a selective role for CCK-B receptors in the control of anxiety. PD134308 and PD135158 are members of a class of anxiolytic agents that have a greatly improved profile compared with benzodiazepines or serotonin-related anxiolytics.
Proglumide is an antagonist but it also blocks CCKA receptors. I'm not sure if that would be a problem or not. The wiki page has some info that would be of interest to opioid addicts:
https://en.wikipedia...wiki/Proglumide
An interesting side effect of proglumide is that it enhances the analgesia produced by opioid drugs,[5] and can prevent or even reverse the development of tolerance to opioid drugs.[6][7] This can make it a useful adjuvant treatment to use alongside opioid drugs in the treatment of chronic pain conditions such as cancer, where opioid analgesics may be required for long periods and development of tolerance reduces clinical efficacy of these drugs.[8][9]
Heres one of the references:
Exogenous cholecystokinin selectively antagonizes opiate analgesia, which suggests that endogenous cholecystokinin may act physiologically as an opiate antagonist and may play a role in opiate tolerance. The use of the selective cholecystokinin antagonist proglumide provided a test of these hypotheses in rats that were either inexperienced with or tolerant to opiates. Proglumide potentiated analgesia produced by morphine and endogenous opiates and seemed to reverse tolerance. These results suggest that endogenous cholecystokinin systems oppose the action of opiates.
Heres a selective CCK-B antagonist:
https://en.wikipedia.org/wiki/CI-988
I have never seen CCK-B antagonists be discussed in threads on addiction. It seems they're well worth looking into, especially for opioid addiction.CI-988 (PD-134,308) is a drug which acts as a cholecystokinin antagonist, selective for the CCKB subtype. In animal studies it showed anxiolytic effects[1][2] and potentiated the analgesic action of both morphine[3] and endogenous opioid peptides,[4][5] as well as preventing the development of tolerance to opioids[6][7] and reducing symptoms of withdrawal.[8][9]
I think selective CRF-1 antagonists may be easier to obtain.
dionysus.psych.wisc.edu/lit/articles/ValdezG2006a.pdf
Development of CRF1 Receptor Antagonists as Antidepressants and Anxiolytics
Depression and anxiety disorders are highly prevalent forms of mental illness
that are considered to be stress-related disorders because some form of stressful
life event often triggers their symptoms. Corticotropin-releasing factor (CRF) is a
41-amino-acid neuropeptide involved in mediating neuroendocrine, autonomic
and behavioural responses to stress, and clinical studies provide evidence for the
role of CRF in the development of depression and anxiety disorders. Two CRF
receptor subtypes have been identified to date – the CRF1 receptor and the CRF2
receptor. Preclinical models provide evidence of a role for CRF1 receptors in the
activation of the stress response. Data from these experiments suggest that
antagonism of CRF1 receptor activity may provide an effective pharmacological
treatment for stress-related psychiatric disorders.
This review highlights progress to date with the development of CRF1 receptor
antagonists as potential pharmacotherapies for depression and anxiety disorders.
Although additional research is needed to fully investigate the efficacy and safety
profiles of CRF1 receptor antagonists as candidate medications for these disor-
ders, the results of preclinical experiments and clinical trials are encouraging.
Further development of these compounds is warranted.
https://en.wikipedia...wiki/Antalarmin
https://en.wikipedia...iki/Pexacerfont
Pexacerfont is a recently developed CRF-1 antagonist which is currently in clinical trials for the treatment of anxiety disorders,[2] and has also been proposed to be useful for the treatment of depression and irritable bowel syndrome.[3]
If anyone needs to see a full article, tell me and I'll see if I can get it for free through my university account.
Edited by mycotheologist, 19 September 2012 - 08:05 PM.
#118
Posted 19 September 2012 - 08:29 PM
http://www.ncbi.nlm....pubmed/15334174
mGlu5 receptor antagonists: a novel class of anxiolytics?
In the early 1990s, a new family of receptors were cloned that were found to mediate the intracellular metabolic effects of glutamate via coupling to secondary messenger systems, that is, the metabotropic glutamate (mGlu) receptors. Eight such receptors (mGlu1 to mGlu8) have been cloned to date, and according to their amino acid sequence, pharmacology and second-messenger coupling, these receptors have been clustered into three groups (I-III). In contrast to the glutamate-gated ion channels (NMDA, AMPA and kainate receptors), which are responsible for fast excitatory transmission, mGlu receptors have been shown to play a modulatory role in the glutamatergic synaptic transmission either by modulating the ion channel activity or by influencing neurotransmitter release. Given the fact that the mGlu receptors are G-protein- coupled, they obviously constitute a new attractive group of "drugable" targets for the treatment of various CNS disorders. The recent discovery of small molecules that selectively bind to receptors of group I (mGlu1 and mGlu5) and group II (mGlu2 and mGlu3) allowed significant advances in our understanding of the roles of these receptors in brain physiology and pathophysiology. The identification of MPEP (2-methyl-6-(phenylethynyl)-pyridine), a highly selective and brain-penetrant mGlu5 receptor antagonist, allowed the exploration of the therapeutic potential of this class of compounds. Subsequent behavior studies revealed that--with the exception of benzodiazepines--mGlu5 receptor antagonists exhibit the widest and most robust anxiolytic activity in preclinical models seen to date. Upcoming clinical studies will soon indicate if the preclinical anxiolytic-like efficacy translates into anxiolytic activity in humans.
And another one is neuropeptide y agonists:
intramural.nimh.nih.gov/research/pubs/crawley06.pdf
Neuropeptide Y (NPY) and galanin (GAL) are densely localized in brain regions subserving stress, fear and anxiety. While previous
research supports a role for both neuropeptides in the mediation of rodent emotional behaviors, there is currently a lack of information on the
effects of central administration of NPY and GAL on fear- and anxiety-related behaviors in mice. In the present study, the effects of
intracerebroventricularly administered NPY and GAL were assessed in C57BL/6J mice on a battery of tests for fear- and anxiety-related
behavior. NPY (0.5, 1.0 nmol) produced clear anxiolytic-like effects in the elevated plus-maze and light X dark exploration test, whereas
GAL (0.5, 1.0 nmol) was without effect. NPY (0.5 nmol) also increased locomotor activity in the open field test. In the fear conditioning
paradigm, NPY administered prior to training reduced freezing to context (0.5, 1.0 nmol) and auditory cue (1.0 nmol). Pre-training GAL (0.5
nmol) treatment reduced freezing to context. Taken together, results demonstrate robust effects of centrally-administered NPY, but not GAL,
on anxiety-like behaviors and fear conditioning in mice. These findings provide a basis for future studies of mice with targeted gene
mutations, directed at delineating the anatomical regions and receptor subtypes mediating the effects of NPY and GAL on emotion.
All this info is of little use to the benzo w/d patient if they can't obtain any compounds in these classes of drugs though. I looked into antalarmin (a CRF-1 antagonist) and it is insanely expensive:
http://www.sigmaaldr...A/A8727?lang=en
Maybe it can be obtained for a reasonable price from a Chinese supplier. Theres a product called Milid which contains proglumide. It used to be sold as an anti-ulcer drug but was superceded by modern anti-ulcer drugs (i.e. H2 antagonists and proton pump inhibitors). The product is still available from what I've read.
Edited by mycotheologist, 19 September 2012 - 08:35 PM.
#119
Posted 20 September 2012 - 11:59 PM
#120
Posted 21 September 2012 - 12:06 AM
I am also thinking about Flumazenil treatment. How did you go about getting permission to do it? It is not a common occurrence and I'm assuming you had to go through a Psychiatrist and Neurologist. Could you explain the process to me so that I might start treatment as well?
I look forward to hearing good news from you in the near future. Please post as soon as you can after your first round of treatment.
Also tagged with one or more of these keywords: benzodiazepines, withdrawal, gotu kola, piracetam, bacopa, nootropics, insomina, delusions, depression, brain fog
3 user(s) are reading this topic
0 members, 3 guests, 0 anonymous users