Hello my friends! Welcome to Abstract Wednesday.
Now that we have some basic enhancements established (see the end of this post for a review) we can see the absolutely essential nature of circadian rhythms for health, mood, energy, learning, memory…everything.
We will continue to focus on light, food, exercise, temperature, etc. in future posts but for today I wanted to talk a little bit about something I call ‘circadian supplementation’.
‘Circadian Supplementation’ is supplementation that takes into account the timing rules imposed by the body’s molecular clocks.
Therefore, from now on when supplementing we must take into account the time of onset of the substance, the peak, the timing of the substance within our three meal per day structure, the interaction of the substance with light, etc.
Let me give you a quick example.
Let’s say I was going to supplement with 50mg of caffeine.
I would not take caffeine right when I wake up at 5am because my 12 hour eating window doesn’t begin until 6am.
I also would not take caffeine at any time in between my meals because that would start up my digestive machinery outside of one my three meals per day and throw off my body’s digestive rhythm. (I’ll explain why this is super important in future posts. I never eat snacks between meals nor do I drink anything other than water right after waking up or between meals.)
I also will never take caffeine after lunch since sleep is of utmost importance, caffeine has a 5 to 6 hour half life, and caffiene disrupts sleep efficiency. (I’ll talk more about this later as well.)
Speaking of sleep, we also need to take substances with short enough half lives or a low enough dose so that sleep disruption is not going to occur. (For example, modafinil is going to be a challenge because of its 12 to 15 hour half-life. Not impossible though.)
Back to caffeine…
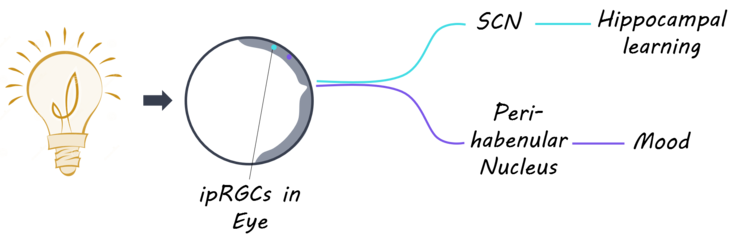
In order to supplement with it I would determine the ‘time to peak’ of caffeine (1 hour), take it with my breakfast at 6am, and then hit my retina with a dose bright light therapy at 7am right when caffeine is hitting it's peak and optimally inhibiting adenosine receptors in the retinohypothalamic tract and enhancing glutamate release into suprachiasmaic nucleus. (see the studies below on caffeine + bright light and also see our reference frame below)
This will help amplify the signal from the retina to the retinal ganglion cells down the RHT to the SCN.
I’ll talk more about this combo later (there are SO many more!) but I just wanted to give you guys a taste of what’s coming.
Long story short, virtually ALL supplements should be taken based on timing rules. (Of course, if you’re prescribed something take it as your doctor recommends!)
Remember, light and sleep (we will always take sleep as a given) are the foundations for everything going forward.
I personally like the light therapy box because it allows me to control dosing and perform timed experiments like the one explained above.
For some reason the glowing hot sphere of nuclear fusion 93 million miles away doesn’t do what I tell it to. The nerve.
Anyway, to give you guys a bit of a road map of what’s ahead, remember that the locus coeruleus sends extensive connections into the hippocampus and prefrontal cortex.
Check this out…

We are going to be headed some crazy places in the next few months.
We now have the perfect starting point for entering the brain (light to the SCN) which branches out to literally every other area of the brain and body from there.
I think of it like initial conditions in chaos theory.
We have 30 trillion human cells and 39 trillion bacterial cells (see study below).
We are trying to synchronize EVERY single one of them perfectly so that the entire superorganism that is us functions to its peak capabilities.
Things are going to be massively unpredictable but if we get the starting point just right…the origin…the 0,0…we just might be able butterfly effect the f#%@ out of the rest of our brain and body and attain our perfectly balanced synchronous optimality.
That’s my goal.
I hope you guys are on board because that’s where we’re headed in the coming weeks and months!
We’re gonna use light to optimize time to optimize life.
We’ve got to walk before we can fly though.
So, with that in mind, here is a (very) partial list of areas I’ve been looking into.
Enjoy!
Levels of Study
Intracellular (nucleus to itself, clock genes)
Organelle to Organelle (mito to mito; mito to nucleus)
Cell to Cell (neuronal primarily but everything)
Set of Cells to Set of Cells (gap junctions in SCN)
Brain Region to Brain Region (neurotransmitters between brain nuclei)
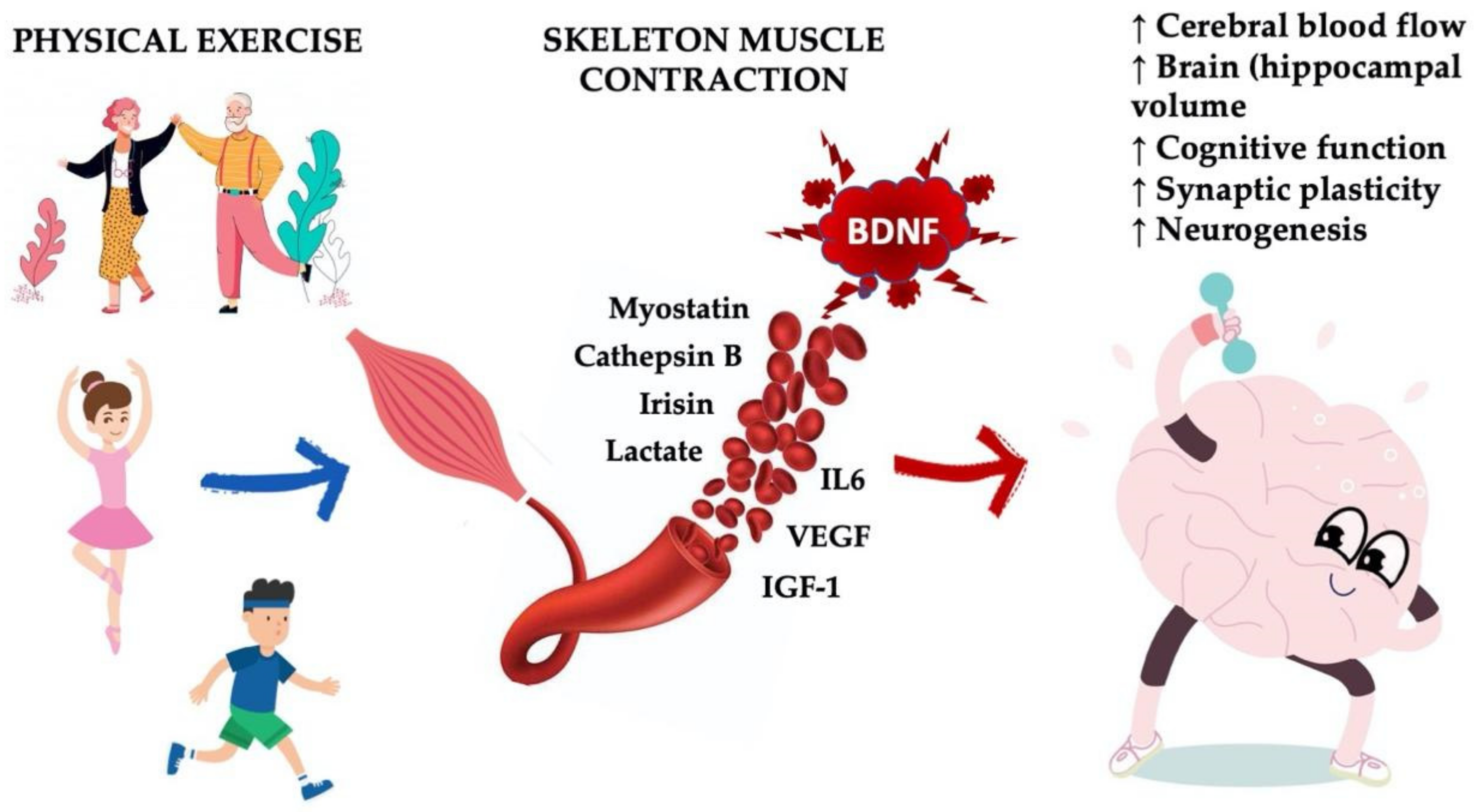
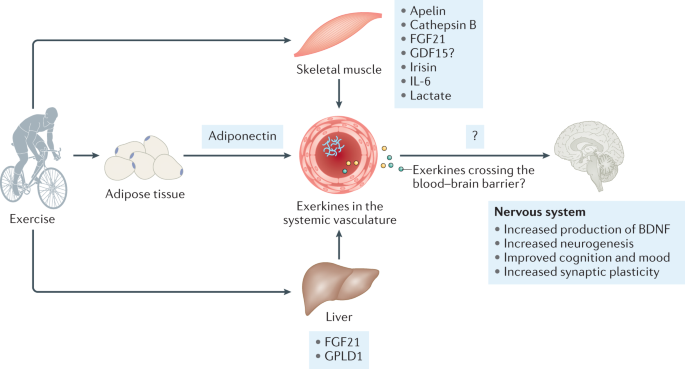
Organ to Organ (exerkines)
Brain to Body (hormones)
Abstracts
Blue Light
https://pubmed.ncbi....h.gov/30674951/
Awakening effects of blue-enriched morning light exposure on university students' physiological and subjective responses
Kyungah Choi 1, Cheong Shin 2, Taesu Kim 1, Hyun Jung Chung 2, Hyeon-Jeong Suk 3
Free PMC article
Abstract
We investigated physiological and subjective responses to morning light exposure of commercially available LED lighting with different correlated colour temperatures to predict how LED-based smart lighting employed in future learning environments will impact students. The classical markers of the circadian system (melatonin and cortisol), as well as the subjective perception of sleepiness, mood, and visual comfort, were compared. Fifteen university students underwent an hour of morning light exposure to both warm (3,500 K) and blue-enriched (6,500 K) white lights at recommended illuminance levels for classrooms and lecture halls (500 lux). The decline of melatonin levels was significantly greater after the exposure to blue-enriched white light. Exposure to blue-enriched white light significantly improved subjective perception of alertness, mood, and visual comfort. With regard to cortisol, we did not find a significant difference in the cortisol decrement between the two light conditions. Our findings suggest that the sensitivity of physiological and subjective responses to white LED light is blue-shifted. These findings, extending the already known effects of short-wavelength light on human physiology, reveal interesting practical implications. Blue-enriched LED light seems to be a simple yet effective potential countermeasure for morning drowsiness and dozing off in class, particularly in schools with insufficient daylight.
https://pubmed.ncbi....h.gov/25559376/
. 2015;58(5):803-10. doi: 10.1080/00140139.2014.983300. Epub 2015 Jan 6.
Blue light aids in coping with the post-lunch dip: an EEG study
Hongchae Baek 1, Byoung-Kyong Min
Abstract
The 'post-lunch dip' is a commonly experienced period of drowsiness in the afternoon hours. If this inevitable period can be disrupted by an environmental cue, the result will be enhanced workplace performance. Because blue light is known to be a critical cue for entraining biological rhythms, we investigated whether blue light illumination can be a practical strategy for coping with the post-lunch dip. Twenty healthy participants underwent a continuous performance test, during which the electroencephalogram (EEG) was recorded under four different illumination conditions: dark ( < 0.3 lx), 33% blue-enriched light, 66% blue-enriched light and white polychromatic light. As a result, exposure to blue-enriched light during the post-lunch dip period significantly reduced the EEG alpha activity, and increased task performance. Since desynchronisation of alpha activity reflects enhancement of vigilance, our findings imply that blue light might disrupt the post-lunch dip. Subsequent exploration of illumination parameters will be beneficial for possible chronobiological and ergonomic applications.
https://pubmed.ncbi....h.gov/25526564/
. 2014 Dec 17;15(12):23448-500. doi: 10.3390/ijms151223448.
Protecting the melatonin rhythm through circadian healthy light exposure
Maria Angeles Bonmati-Carrion 1, Raquel Arguelles-Prieto 2, Maria Jose Martinez-Madrid 3, Russel Reiter 4, Ruediger Hardeland 5, Maria Angeles Rol 6, Juan Antonio Madrid 7
Abstract
Currently, in developed countries, nights are excessively illuminated (light at night), whereas daytime is mainly spent indoors, and thus people are exposed to much lower light intensities than under natural conditions. In spite of the positive impact of artificial light, we pay a price for the easy access to light during the night: disorganization of our circadian system or chronodisruption (CD), including perturbations in melatonin rhythm. Epidemiological studies show that CD is associated with an increased incidence of diabetes, obesity, heart disease, cognitive and affective impairment, premature aging and some types of cancer. Knowledge of retinal photoreceptors and the discovery of melanopsin in some ganglion cells demonstrate that light intensity, timing and spectrum must be considered to keep the biological clock properly entrained. Importantly, not all wavelengths of light are equally chronodisrupting. Blue light, which is particularly beneficial during the daytime, seems to be more disruptive at night, and induces the strongest melatonin inhibition. Nocturnal blue light exposure is currently increasing, due to the proliferation of energy-efficient lighting (LEDs) and electronic devices. Thus, the development of lighting systems that preserve the melatonin rhythm could reduce the health risks induced by chronodisruption. This review addresses the state of the art regarding the crosstalk between light and the circadian system.
https://pubmed.ncbi.nlm.nih.gov/31433569/
. 2019 Dec;12(12):e201900102. doi: 10.1002/jbio.201900102. Epub 2019 Sep 2.
The inner clock-Blue light sets the human rhythm
Abstract
Visible light synchronizes the human biological clock in the suprachiasmatic nuclei of the hypothalamus to the solar 24-hour cycle. Short wavelengths, perceived as blue color, are the strongest synchronizing agent for the circadian system that keeps most biological and psychological rhythms internally synchronized. Circadian rhythm is important for optimum function of organisms and circadian sleep-wake disruptions or chronic misalignment often may lead to psychiatric and neurodegenerative illness. The beneficial effect on circadian synchronization, sleep quality, mood, and cognitive performance depends not only on the light spectral composition but also on the timing of exposure and its intensity. Exposure to blue light during the day is important to suppress melatonin secretion, the hormone that is produced by the pineal gland and plays crucial role in circadian rhythm entrainment. While the exposure to blue is important for keeping organism's wellbeing, alertness, and cognitive performance during the day, chronic exposure to low-intensity blue light directly before bedtime, may have serious implications on sleep quality, circadian phase and cycle durations. This rises inevitably the need for solutions to improve wellbeing, alertness, and cognitive performance in today's modern society where exposure to blue light emitting devices is ever increasing.
Caffeine + Bright Light
https://pubmed.ncbi....h.gov/35398627/
. 2022 May;93:15-25. doi: 10.1016/j.sleep.2022.03.013. Epub 2022 Mar 24.
Bright light alone or combined with caffeine improves sleepiness in chronically sleep-restricted young drivers
Shamsi Shekari Soleimanloo 1, Veronica Garcia-Hansen 2, Melanie J White 3, M Mamun Huda 4, Simon S Smith 4
Abstract
Background: Young drivers are over-involved in sleepiness-related crashes. The alerting effects of bright light offer a potential countermeasure for driver sleepiness, either replacing or in conjunction with current countermeasures such as the use of caffeine.
Methods: Thirty young (18-25) chronically sleep-restricted drivers drove in a simulator under randomized conditions of continuous bright light ('Light,' 500 nm, 230μw/cm2), caffeine ('Caffeine,' 100 mg caffeinated gum), or light and caffeine together ('Light + Caffeine'), after driving under a placebo condition ('Placebo,' decaffeinated gum, 555 nm light, 0.3 μW/cm2) on three consecutive days. Using mixed-effects linear models, the associations between these conditions and physiological outcomes (EEG alpha and theta power, heart rate, and beat-to-beat intervals), driving performance (lateral lane and steering-related outcomes and lateral acceleration), and subjective sleepiness was assessed.
Results: Relative to Placebo, all conditions improved driving performance outcomes (P < 0.0001), with effects of Light + Caffeine equal to Light but greater than Caffeine. Light + Caffeine reduced EEG alpha power more than Light or Caffeine (P < 0.0006), but ECG outcomes were generally worse under all conditions relative to Placebo. Subjective sleepiness improved under the Light + Caffeine condition only (P < 0.0001).
Conclusions: Combining bright light and caffeine enhances their alerting effects on lateral lane variability and subjective sleepiness. A bright light could be a practical alternative to caffeine for sleepy drivers who avoid caffeine. The alerting effects of bright light could alleviate chronic community-level mild sleep restriction and provide on-road benefits to reduce severe injuries and fatal sleepiness-related crashes.
Lithium
https://pubmed.ncbi....h.gov/33650218/
. 2021 Aug;23(5):445-453. doi: 10.1111/bdi.13070. Epub 2021 Mar 16.
Effect of lithium on circadian rhythm in bipolar disorder: A systematic review and meta-analysis
Ni Xu 1, Kiyomi Shinohara 2, Kate E A Saunders 1 3, John R Geddes 1 3, Andrea Cipriani 1 3
Abstract
Objectives: Circadian rhythm disruption is commonly reported in patients with bipolar disorder. Lithium has been suggested to have effects on the circadian clock, the biological basis of the circadian rhythm. The objective of the current review was to review systematically the existing studies on the effect of lithium on circadian rhythm in patients with bipolar disorder.
Methods: We systematically searched the scientific literature up to September 2020 for experimental or observational studies which measured circadian rhythm in bipolar patients taking lithium (in comparison with placebo or other active treatments) and carried out a meta-analysis. Circadian rest-activity was our primary outcome, but we also collected data about sleep quality and chronotype (Morningness-Eveningness). The protocol was registered in PROSPERO (CRD42018109790).
Results: Four observational studies (n = 668) and one experimental study (n = 29) were included. Results from the meta-analysis suggest a potential association between lithium and shifts towards morningness (standardized mean difference [SMD]: 0.42, 95% confidence interval [CI]: -0.05 to 0.90). One cohort study with 21 days of follow-up found that patients treated with lithium had significantly larger amplitude (0.68, 0.01 to 1.36) when compared to anticonvulsants.
Conclusion: This review highlights the insufficient evidence to inform us about the effect of lithium on circadian rhythm. However, we found that chronotype can be a potential target for further exploration of biomarkers or biosignatures of lithium treatment in patients with bipolar disorder. Further studies with prospective and longitudinal study design, adopting actigraphy to monitor daily circadian rest-activity changes are needed.
Bright Light Therapy + Methylphenidate (Ritalin/Concerta) + Melatonin
. 2021 Jun;11(2):170-179. doi: 10.1136/bmjspcare-2019-001877. Epub 2020 Jan 10.
Sleep disturbance in patients with cancer: a feasibility study of multimodal therapy
Sriram Yennurajalingam 1, Cindy Carmack 2, Dave Balachandran 3, Cathy Eng 4, Bora Lim 5, Marvin Delgado 2, Diana Guzman Gutierrez 2, Monica Raznahan 2, Minjeong Park 6, Kenneth R Hess 6, Janet L Williams 2, Zhanni Lu 2, Jewel Ochoa 2, Eduardo Bruera 2
Abstract
Background: Our aim was to determine feasibility and effect sizes of bright light therapy (BLT), melatonin (MLT), methylphenidate (MP) and eight combinations (BLT+MLT+MP, BLT+MLT, BLT+MP, BLT alone, MLT+MP, MLT alone, MP alone, placebo for BLT, MLT and MP) defined as multimodal therapy (MMT), to improve sleep quality (SQ) (Pittsburgh Sleep Quality Index (PSQI)) from baseline to day 15. We also examined the effects of MMT on insomnia, fatigue, depression, quality of life and actigraphy.
Methods: Patients with advanced cancer with poor SQ (PSQI ≥5) were eligible. Using a double-blind randomised factorial study design, patients were randomised into 1 of the 8 arms for 2 weeks. Feasibility and effect sizes were assessed.
Results: 81% (54/67) of randomised patients completed the study. There were no differences in the demographics and SQ between groups. The adherence rates for BLT, MLT and MP were 93%, 100% and 100%, respectively. BLT+MLT+placebo of MP; BLT+placebo of MLT+placebo of MP; BLT+MLT+MP showed an effect size (Cohen's d) for change in PSQI scores of 0.64, 0.57 and 0.63, respectively. PSQI change using linear regression showed BLT (n=29) has effect size of 0.46, p=0.017; MLT (n=26), 0.24, p=0.20; MP (n=26), 0.06, p=0.46. No significant differences were observed in scores for insomnia, fatigue, depression, quality of life and actigraphy. There were no differences in adverse events by groups(p=0.80).
Conclusions: The use of MMT to treat SQ disturbance was feasible. BLT+MLT showed the most promising effect size in improvement in SQ, and additional larger studies are needed.
Human Cells vs. Bacterial Cells
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4991899/
PLoS Biol. 2016 Aug; 14(8): e1002533.
Published online 2016 Aug 19. doi: 10.1371/journal.pbio.1002533
Revised Estimates for the Number of Human and Bacteria Cells in the Body
Ron Sender,1 Shai Fuchs,2,¤* and Ron Milo1,*
Author information Copyright and License information Disclaimer
Abstract
Reported values in the literature on the number of cells in the body differ by orders of magnitude and are very seldom supported by any measurements or calculations. Here, we integrate the most up-to-date information on the number of human and bacterial cells in the body. We estimate the total number of bacteria in the 70 kg "reference man" to be 3.8·1013. For human cells, we identify the dominant role of the hematopoietic lineage to the total count (≈90%) and revise past estimates to 3.0·1013 human cells. Our analysis also updates the widely-cited 10:1 ratio, showing that the number of bacteria in the body is actually of the same order as the number of human cells, and their total mass is about 0.2 kg.
Dopamine
. 2017 Aug 21;27(16):2465-2475.e3. doi: 10.1016/j.cub.2017.06.084. Epub 2017 Aug 3.
Direct Midbrain Dopamine Input to the Suprachiasmatic Nucleus Accelerates Circadian Entrainment
Ryan M Grippo 1, Aarti M Purohit 1, Qi Zhang 1, Larry S Zweifel 2, Ali D Güler 3
Free PMC article
Abstract
Dopamine (DA) neurotransmission controls behaviors important for survival, including voluntary movement, reward processing, and detection of salient events, such as food or mate availability. Dopaminergic tone also influences circadian physiology and behavior. Although the evolutionary significance of this input is appreciated, its precise neurophysiological architecture remains unknown. Here, we identify a novel, direct connection between the DA neurons of the ventral tegmental area (VTA) and the suprachiasmatic nucleus (SCN). We demonstrate that D1 dopamine receptor (Drd1) signaling within the SCN is necessary for properly timed resynchronization of activity rhythms to phase-shifted light:dark cycles and that elevation of DA tone through selective activation of VTA DA neurons accelerates photoentrainment. Our findings demonstrate a previously unappreciated role for direct DA input to the master circadian clock and highlight the importance of an evolutionarily significant relationship between the circadian system and the neuromodulatory circuits that govern motivational behaviors.
Our Enhancements So Far:
1. Sync Your Central Clock with Bright Light Therapy: Go to bed at the same time every day and wake up at the same time every day. Do 30 minutes of bright light therapy first thing in the morning to sync your master circadian clock. Resync your master circadian clock and enhance melatonin secretion with 30 minutes of midday bright light therapy. Click here for my recommended bright light device. http://www.lostfalco...re-to-buy-them/
2. Sync Your Microbiome Clock with Dextrin: Eat fiber at the beginning of each meal to sync your microbiome clock. Click here to try dextrin. https://www.lostfalco.com/supplements/
3. Sync Your Peripheral Clock with Meal Timing and Exercise Timing (Hex Bar, Pull Up Bar, Fit Desk): Eat at the same times each day within an 8 to 12 hour window and exercise for 30 min (remember the exerkines!) at the same time every day. Click here for simple, affordable devices you can use at home. https://www.lostfalco.com/devices/
4. Use 'Sequence Eating' to Control Glycemic Response: Eat Fiber/Veggies first THEN Protein THEN Carbs (eat fat with fiber and/or protein) https://www.lostfalco.com/supplements/
Our Reference Frame
Edited by lostfalco, 27 November 2022 - 04:43 PM.