Discussion
The molecular events leading to inflammatory arthritis are complex and involve a number of factors. Some studies have implicated MC in arthritis, and preventing mediator release from these cells has become a target for therapeutic intervention [11,53]. The initial impetus for these studies was the observation that certain fullerene derivatives can stabilize MC in vitro and in vivo. In the present studies, we confirmed that fullerenes could partially limit MC activation in vitro, an effect associated with specific derivitzation of the nanoparticles. Interestingly, while these compounds proved moderately effective in immune complex-driven K/BxN serum transfer arthritis, this effect was not fully attributable to MC inhibition, because the agents retained modest but discernable effect in MC-deficient Cre-Master mice. Consistent with this result, fullerenes manifested in vitro effects of a potentially anti-inflammatory nature on other lineages implicated in arthritis: fibroblasts and osteoclasts. However, in the more complex CIA model, the fullerene effect was no longer discernable, despite recent evidence (in the B6 background) for a role of MC in this model [51], which may be further explained by the model of arthritis induction and future experiments will be directed towards such studies, including using the CIA model in the MC-deficient mice.
The strategy for these studies was to first determine which fullerene derivatives inhibited human and mouse MC through arthritis–relevant stimulation. In addition, the ability of fullerene derivatives to inhibit synovial fibroblast cytokine production and osteoclast development were considered important prerequisites for predicting in vivo efficacy, as an amalgam of cell types govern the degree and severity of arthritis [19,54]. To this end, a panel of fullerene derivatives were tested for their ability to inhibit MC FcγR-mediated responses [55]. A clear structure-activity relationship between fullerene derivatives and inhibitory function was not defined. However, in general, the fullerene derivatives that were most efficient at inhibiting MC mediator release had side chain moieties that induced maximum water solubility, a zeta potential between 37 and -146 mV, and particle sizes between 50 to 200 nM. Of these, both TGA and ALM have been shown previously to inhibit IgE-mediated degranulation and cytokine production [25] and in response to other non-IgE-mediated secretagogues [46]. The TGA (tetra-glycolic acid) is a C70 series with four carboxyl groups, which confers water solubility. It is postulated that the mechanism by which TGA exerts its effect via an interaction between the carboxyl groups and the electrons on the fullerene cage. To examine this point, a similar fullerene derivative that presented a triethylene glycol spacer between the carboxyl groups and the cage was prepared. TEG-TGA (-25 mV zeta potential; 94 nM particle size) did not block MC mediator release nor did it interfere with cytokine release (not shown). This result is consistent with the hypothesis that proximity of the carboxyl groups to the cage is necessary for activity.
The mitochondrial electron transport is the machinery that orchestrates one of the most fundamental of chemical processes; the generation of cellular energy from oxygen resulting in the fuel that supports all eukaryotic life. However, it is a highly sensitive process and, unbalanced, leads to the generation of free radicals or ROS which have been linked as a mechanism underlying many chronic human diseases including MC activation and inflammatory arthritis [56,57]. ALM is a mitochondria- targeting fullerene derivative that has been previously shown to home to mitochondria and inhibit inflammation [27,28]. ALM was designed to accumulate in the internal mitochondrial membrane bilayers positioned to neutralize superoxide molecules, reactive lipid radicals, and radicals that have formed on transmembrane proteins at the site where they are generated. Subsequently, this is predicted to impact diseases whose pathologies stem from radical injury.
To this end both fullerene derivatives significantly block ROS production and mitochondrial membrane potential. While it has been shown previously that human MC degranulation in response to FcεRI and Fcγ-signaling involves ROS [58,59], it is not clear if blocking ROS directly blocks degranulation and cytokine production. Results here suggest that blocking ROS using ALM and TGA in response to IC (an FcγRIIA-dependent stimuli [35]) parallels inhibition of mediator release. This is in line with previous work suggesting that fullerenes interfere with the generation of mitochondrial-derived ROS [60–63]. It is also demonstrated that mitochondrial membrane potential is a critical determinant in human MC FcγR-mediated degranulation. While further studies are needed these data suggest that fullerenes inhibit MC through a mechanism involving the mitochondrial membrane potential and suggest a role of the mitochondria in human MC non-IgE mediator release.
Nuclear factor-kappa B is involved in the pathophysiology of inflammatory and efforts to target its function through molecular targets in the pathway leading to its activation are underway [64–66]. This transcription factor induces both TNF-α and IL-1β gene expression which can both in turn activate the NF-κB pathway inducing an autocrine loop which perpetuates inflammation. Interestingly, some of the drugs for RA were shown to block either the NF-κB activation cascade or its action [64,65,67]. For example, gold-containing therapeutics, TNF-α inhibitors, and methotrexate, all regularly used for treating arthritis, can effect NF-κB function [68–70]. Several fullerene derivatives, including ALM and TGA, inhibited IC-induced NF-κB activation in human MC. Current studies are examining what signaling molecules in the ROS/TNF/NF-κB pathway [49] are affected by fullerene derivatives.
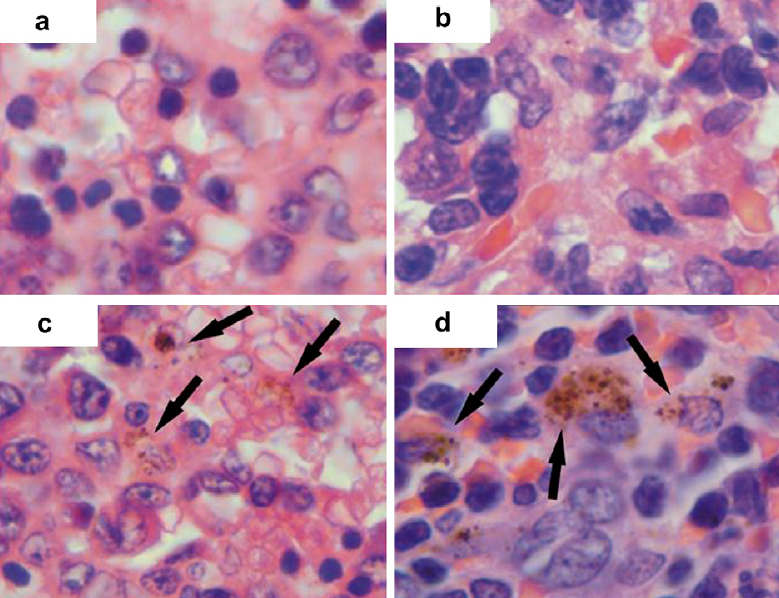
Arthritic joint tissues demonstrate a striking predilection for uptake of ALM. Indeed, this strong uptake may provide a partial basis for their efficacy in ameliorating K/BxN arthritis. It was also demonstrated that fullerene derivatives inhibited the onset of arthritis in K/BxN serum transfer arthritis in C57Bl/6 mice. There was a small but not significant improvement in the CIA model. The K/BxN serum transfer model induces a rapid and severe synovitis dependent on neutrophils, MC, and macrophages. A role for MC in this system had also been proposed by studies in mice that lack MC on the basis of mutations affecting the Kit-KitL (stem cell factor) axis (W/Wv,Sl/Sld, and Pretty2) [29,33]. These mice are resistant to disease induction following serum transfer, and susceptibility can be restored by MC engraftment. However, studies in Kit-independent models of MC deficiency have not found an effect on arthritis in this model, suggesting that the phenotype of Kit-mutant mice may reflect the role of stem cell factor on lineages beyond the MC [50]. In the Cre-Master mice employed here, MC deficiency results through a genotoxicity from high levels of Cre recombinase driven by the carboxypeptidase A3 locus, resulting in Trp53-dependent MC depletion. Whereas Cre-Master still exhibit some residual arthritis inhibition by fullerenes, our data suggested that MC are not the only relevant target of fullerenes in this system. Given the differences in MC phenotypes and expression between the rodent and human systems [71], further studies are needed to determine whether the effect of fullerenes on MC represents an interesting strategy for intervention in human arthritis.
As in other studies using purified and well characterized fullerene derivatives [25,26,72–74], no liver or kidney toxicity was detected using repeated dosing of concentrations higher than that needed for in vivo efficacy. The in vivo imaging studies also demonstrated a lack of uptake in other organs, which portends well for a favorable toxicity profile in clinical development of ALM. More advanced toxicity studies would be needed to assess these two fullerene derivatives before moving forward with human application.
In conclusion, it was demonstrated that not all fullerene derivatives exhibit the same ability to inhibit inflammatory mediator release from MC and synovial fibroblasts. Two fullerene derivatives were able to significantly block the onset of serum-induced arthritis in vivo leading to a blunted inflammatory response; however CIA-induced mice were refractory to fullerene treatment. More studies are needed to identify those structure-activity relationships that are dependent on the moieties added to the fullerene carbon cage in order to define the precise mechanism by which these fullerene derivatives inhibit inflammatory disease.