It makes more sense to improve vitamin C effectiveness than going to absurdly high dosages, I might suggest liposomal as a much smarter and cheaper way to go.
Maybe smarter, but definitely not cheaper. My daily 20g in divided doses costs me merely 0,40 cents.
The following paper is now behind a paywall, but questions the usual notion that vitamin C serum levels would reach their upper limit already with dietary intake of 250-500 mg at about 50-100 µM (concluded by giving doses up to 2.5 g, and extrapolated for all higher doses). While actually measuring serum levels with 20g/d yielded even above 500 µM.
Journal of the New Zealand Medical Association, 23-August-2002, Vol 115 No 1160
Glycohaemoglobin and ascorbic acid
Copplestone et al1 (http://www.nzma.org....al/115-1157/25/) identified misleading glycohaemoglobin (GHb) results due to a haemoglobin variant (Hb D Punjab) and listed a number of other possible causes for such false results (ie, haemolytic anaemia, uraemia, lead poisoning, alcoholism, high-dose salicylates and hereditary persistence of foetal haemoglobin).
We have observed a significant "false" lowering of GHb in animals and humans supplementing ascorbic acid (AA) at multigram levels. Mice receiving ~7.5 mg/d (equivalent to > 10 g/day in a 70 kg human) exhibited no decrease in plasma glucose, but a 23% reduction in GHb.2 In humans, supplementation of AA for several months did not lower fasting plasma glucose.3,4 We studied 139 consecutive consenting non-diabetic patients in an oncology clinic. The patients had been encouraged as part of their treatment to supplement AA. Self-reported daily intake varied from 0 to 20 g/day. The plasma AA levels ranged from 11.4 to 517 µmol/L and correlated well with the reported intake. Regression analysis of their GHb and plasma AA values showed a statistically significant inverse association (eg, each 30 µmol/L increase in plasma AA concentration resulted in a decrease of 0.1 in GHb).
A 1 g oral dose of AA can raise plasma AA to 130 µmol/L within an hour and such doses at intervals of about two hours throughout the day can maintain ~230 µmol AA/L.5 Similar levels could also be achieved by use of sustained-release AA tablets. This AA concentration would induce an approximate 0.7 depression in GHb. The GHb assay used in our study, affinity chromatography, is not affected by the presence of AA.3 Thus, unlike the case with Hb D Punjab, our results were not caused by analytical method artifact. More likely, the decreased GHb associated with AA supplementation appears related to an in vivo inhibition of glycation by the elevated plasma AA levels, and not a decrease in average plasma glucose.3 If this is true, the effect has implications not only for interpretation of GHb but also for human ageing, in which glycation of proteins plays a prominent role in age-related degenerative changes.
A misleading GHb lowering of the magnitude we observed can be clinically significant. Current recommendations for diabetics suggest that GHb be maintained at 7, a level that is associated with acceptable control and decreased risk of complications; when GHb exceeds 8, re-evaluation of treatment is necessary.6 Moreover, relatively small increases in average blood sugar (ie, GHb) can accompany adverse reproductive effects. A difference in mean maternal GHb of 0.8 was found for women giving birth to infants without or with congenital malformations.7 In either of these circumstances, an underestimation of GHb could obscure the need for more aggressive intervention.
Vitamin usage is common in New Zealand and after multivitamins, AA is the most often consumed supplement.8 Moreover, diabetics are encouraged to supplement antioxidants, including AA. Thus, it seems prudent for primary care health providers to inquire regarding the AA intake of patients, especially diabetics, when using GHb for diagnosis or treatment monitoring.
Cheryl A Krone
Senior Research Scientist
John TA Ely
Director
Applied Research Institute
PO Box 1925
Palmerston North
References:
- Copplestone S, Mackay R, Brennan S. Normal glycated haemoglobin in a patient with poorly controlled diabetes mellitus and haemoglobin D Punjab: implications for assessment of control. NZ Med J 2002;115(1157). URL: http://www.nzma.org....al/115-1157/25/
- Krone CA, Ely JTA. Vitamin C and glycohemoglobin revisited. Clin Chem 2001;47(1):148.
- Davie SJ, Gould BJ, Yudkin JS. Effect of vitamin C on glycosylation of proteins. Diabetes 1992;41(2):167–73.
- Paolisso G, Balbi V, Bolpe C, et al. Metabolic benefits deriving from chronic vitamin C supplementation in aged non-insulin dependent diabetics. J Am Coll Nutr 1995; 14(4):387–392.
- Lewin S. Vitamin C: Its Molecular Biology and Medical Potential. New York: Academic Press; 1976.
- Kenealey T, Braatvedt G, Scragg R. Screening for type 2 diabetes in non-pregnant adults in New Zealand: practice recommendations. NZ Med J 2002;115(1152):194–6.
- Rosenn B, Miodovnik M, Dignan PS, et al. Minor congenital malformation in infants of insulin-dependent diabetic women: association with poor glycemic control. Obstet Gynecol 1990;76:745–9.
- Allen T, Thomson WM, Emmerton LM, Poulton R. Nutritional supplement use among 26-year-olds. N Z Med J 2000;113(1113):274–7.
The problem is that actual serum levels on high dose oral vitamin C are rarely measured. Except maybe in the following case studies, comparing different doses of ascorbic acid with lipsomal:
Though a bid strange, since they compared 5 gram of regular oral ascorbic acid to 20g or 36g liposomal - in that resulting plasma levels of initial equal oral doses (5g) showed almost identical!
Pharmacokinetics of oral vitamin C
STEPHEN HICKEY, HILARY J. ROBERTS, & NICHOLAS J. MILLER
"Figure 1 shows the response of the female subject to single 5 g doses of liposomal and
standard formulation vitamin C; both produced similar response curves. These results are
comparable in form and magnitude to those expected for oral vitamin C in previously
depleted subjects. However, peak values exceeded 220 mM L which has been reported as
the maximum value attainable with repeated oral doses of 3 g six times daily [8]. The
subjects were experienced users of high-dose vitamin C and neither suffered any
gastrointestinal effects at this dose level.5 "
Increasing the dose of liposomal vitamin C to 20g gave a broader response, with
a delayed maximum, as shown in Figure 2. In this graph, the 20g liposomal dose is
compared with a 5g standard dose (male subject). With a 20g intake, the peak plasma
level was delayed and the response was broader, indicating a greater absorption of
vitamin C. The 5g data set shows a marked outlier (peak): this is attributed to the fact
that one of the (5g) blood samples was difficult to extract, with inflammation at the
puncture site, providing only a small sample. The subject experienced no bowel
tolerance effects at either of these intakes.
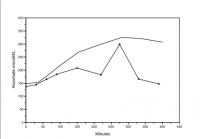
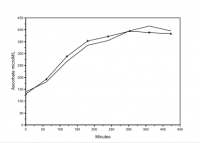
Figure 3 shows plasma levels following a 36g dose of liposomal vitamin C, for
both subjects. This resulted in peak plasma levels, in the region of 400 µM/L. A 95%
interfractile range (34-114), which contains 95% of the distribution with a mean of 74
corresponds to a calculated standard deviation of 17.4. We note that, under these
conditions, an outlier measurement of 400 µM/L would correspond to a deviation of
10.3 σ with a theoretical p value of 1.6x10 -13 (i.e. P<0.0000000000001). With this high
dose, both subjects exceeded their bowel tolerance, leading to diarrhoea. This
intolerance presumably arose from the high intake of phospholipid, without food
buffering, in fasting individuals. However, our observations using hourly doses suggest
that daily intakes of this magnitude are tolerable without bowel effects, as long as the
dose is spread throughout the day.
However, these graphs only tell about serum levels, not how much actually entered cells. Where thel real strength of liposomal would show.
Some suggest the best strategy in bad health would be a combination of regular oral ascorbic acid, mineral ascorbates, ascorbyl palmitate and liposomal vitamin C combined.
But my budget not permitting, I'm already glad about the results of normal vitamin C reported in an other post 3 years ago:
My personal beneficial experiences with mega-dosing Vitamin C is related in this post already:
- Vitamin C (after a PAD diagnosis almost 5 years ago, together with lysine and all other nutrients recommended by Linus Pauling) - pain-free walking distance improved from mere 3-400 meters up to 2 hours. But only once I exceeded the in his view minimal therapeutic dose of 6g/d. Side-benefits: a since 2 years persistent skin-rush cleared up, hay-fewer symptoms recurring every spring since 12 years got alleviated (though this year it took 30 g/d; in avg. about 20 g/d for 5 years). HbA1c stayed unproportionally low, compared to rising blood glucose. Truly addictive stuff for someone with my health-issues. Only negative side-effect: flatulence.
- ...